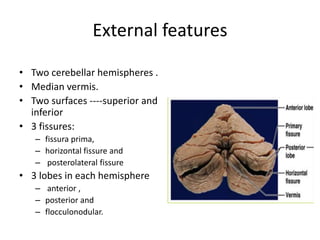
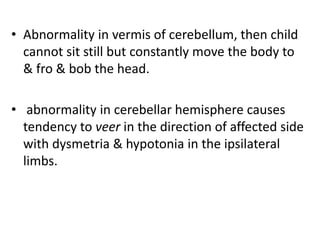
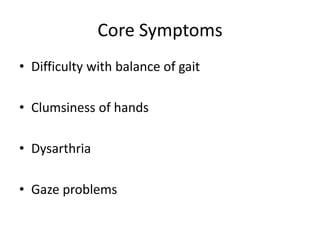
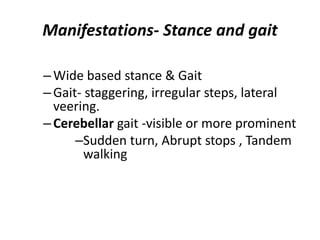
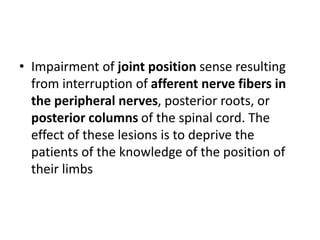
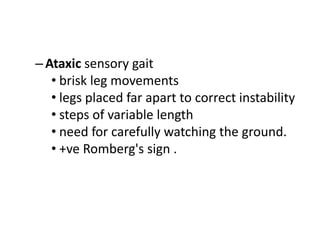
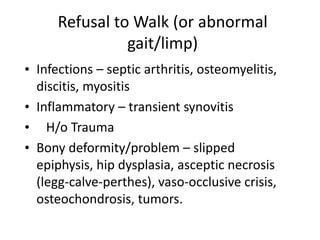
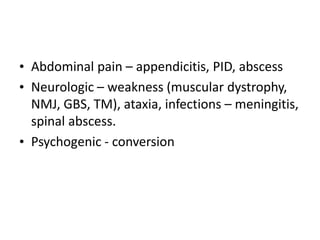
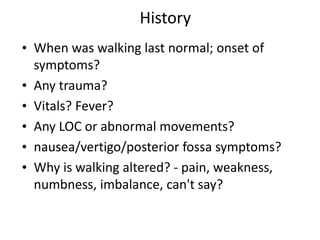
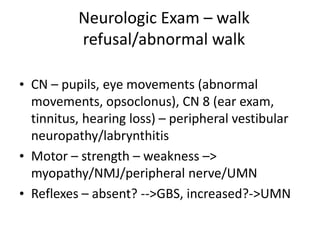
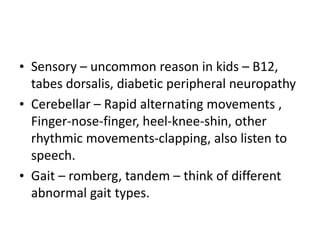
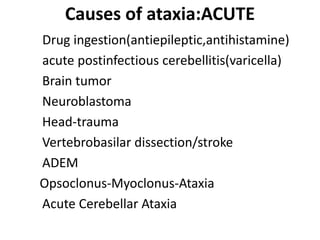
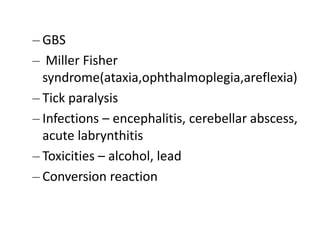
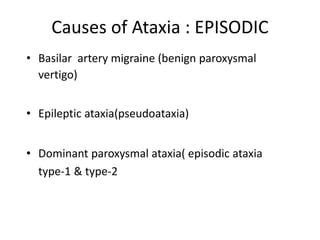
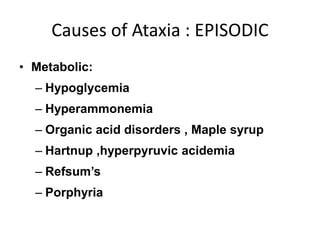
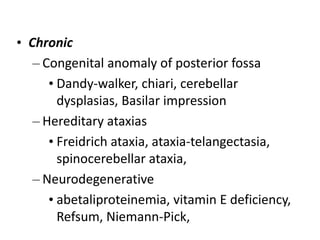
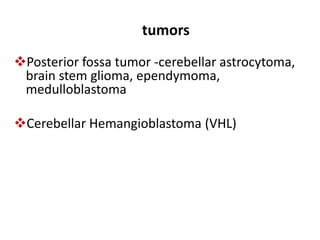
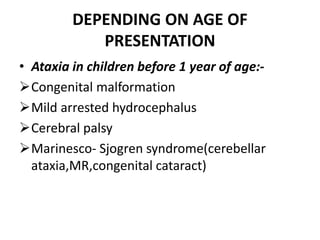
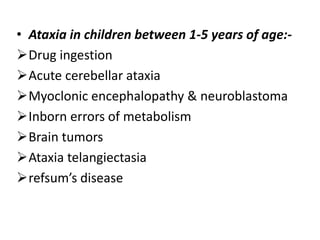
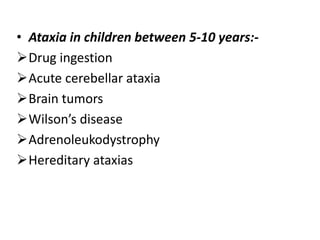
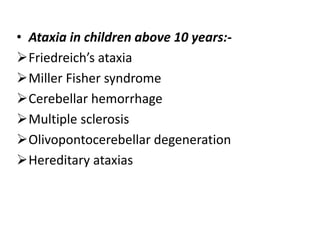
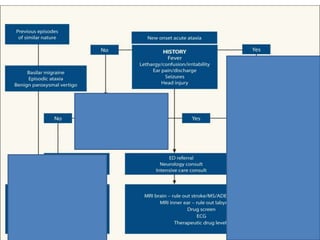
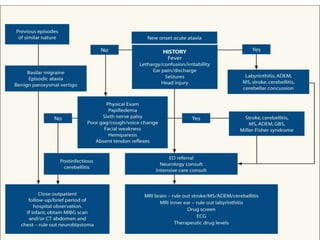
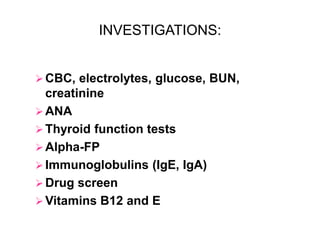
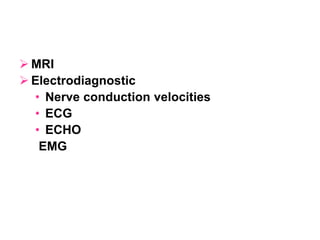
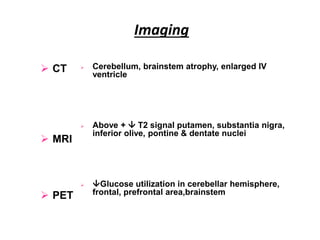
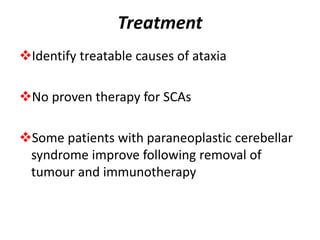
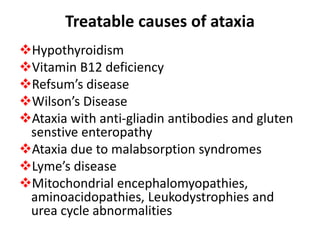
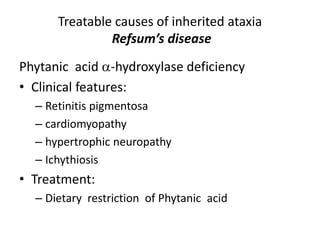
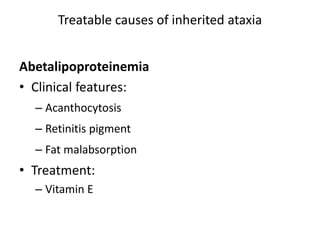
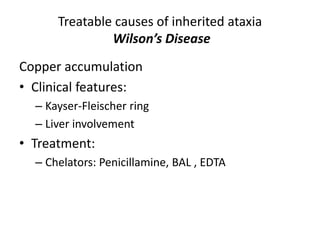
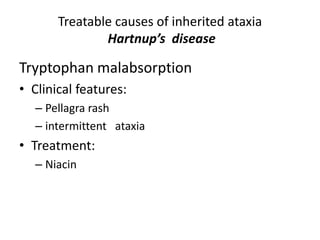
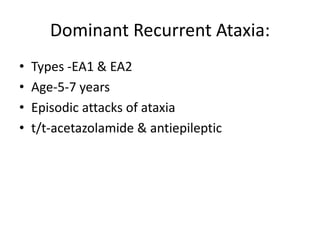
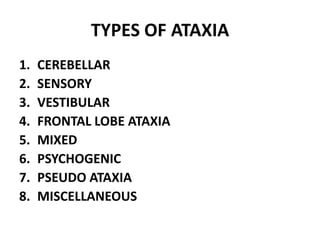
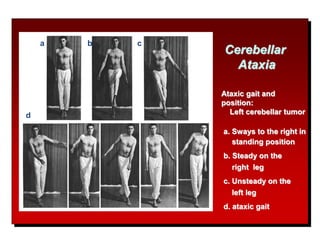
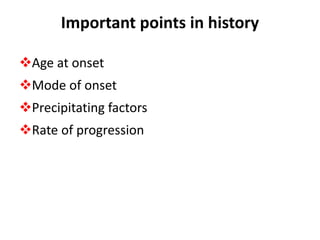
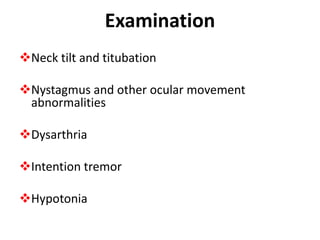
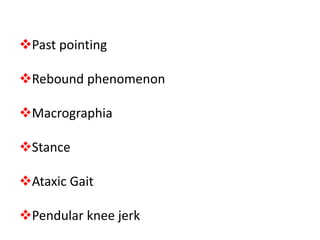
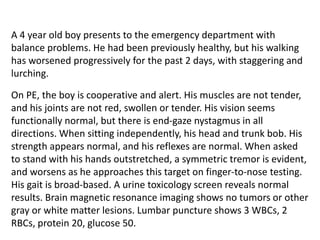
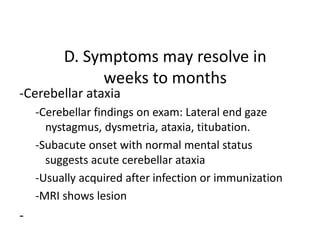
Ataxia is a symptom of poor coordination of movement that can affect walking, fingers, speech, and eye movements. It is caused by abnormalities in the cerebellum which coordinates movement. The document discusses various types and causes of ataxia including acute, episodic, chronic, and hereditary forms. Imaging and investigations help identify treatable causes while most hereditary ataxias currently have no proven treatment.