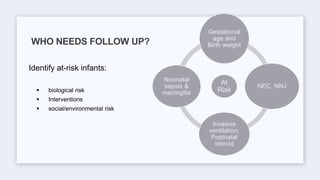
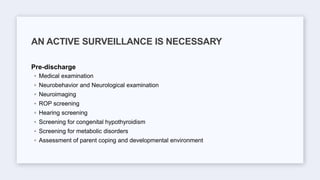
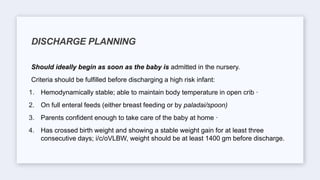
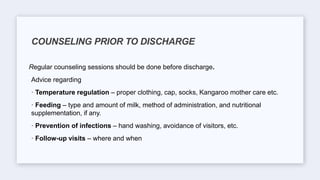
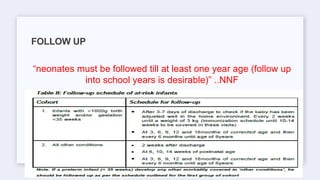
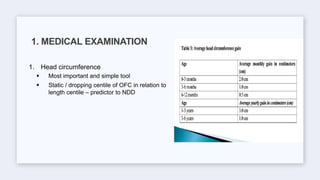
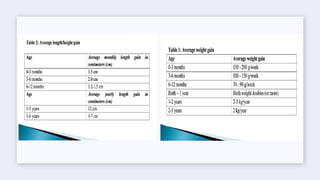
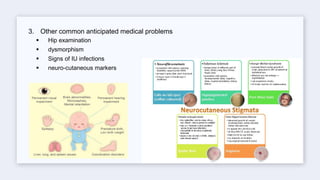
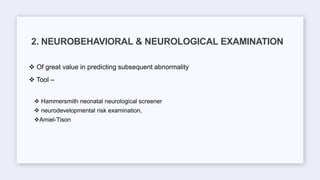
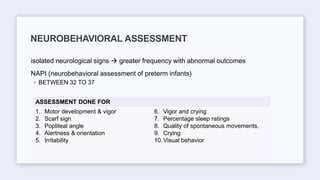
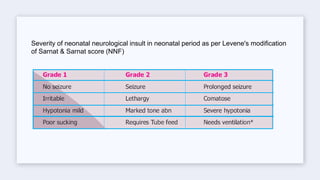
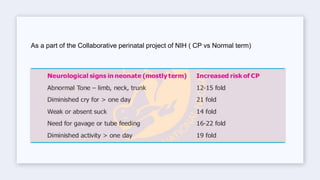
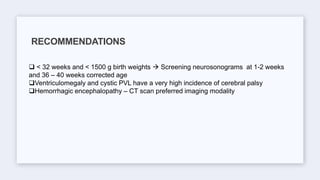
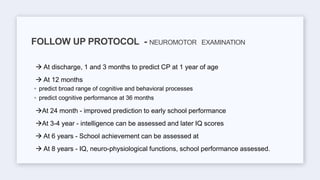
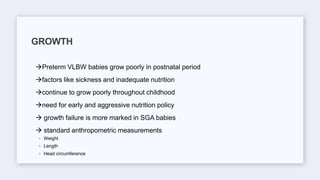
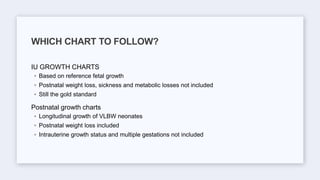
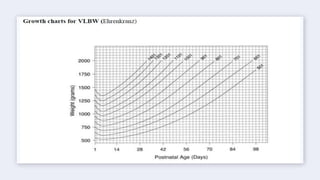
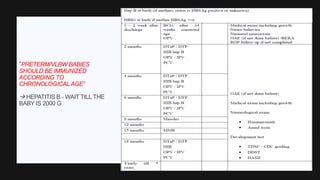
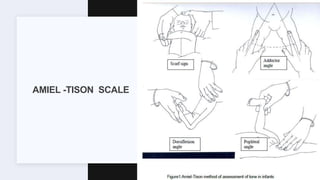
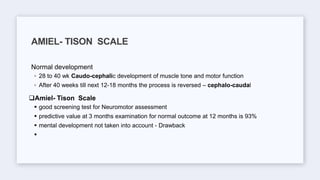
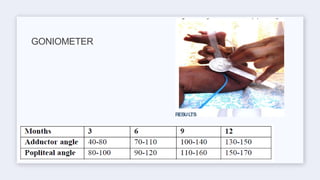
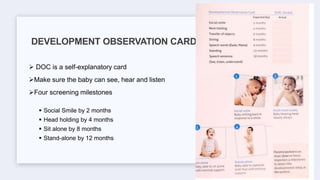
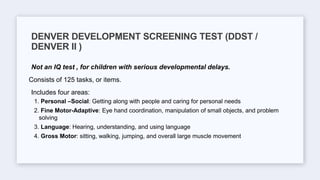
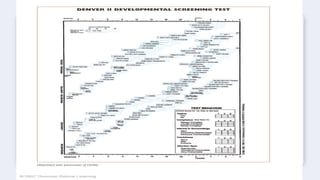
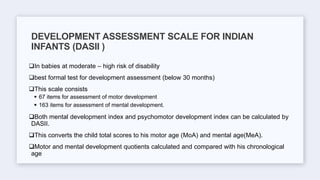
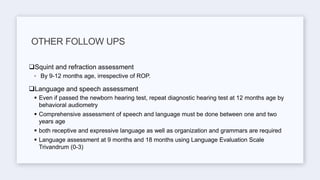
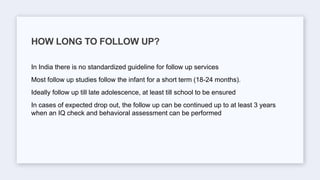
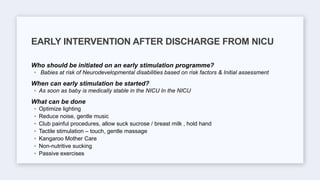
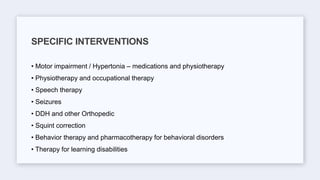
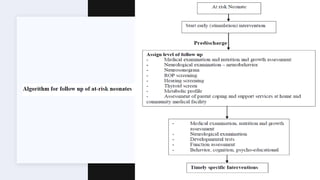
This document discusses the importance of follow-up care for high-risk newborns after discharge from the NICU. It outlines that follow-up should include regular medical examinations to monitor growth and development, screening tests, and neurobehavioral assessments. Follow-up care is most intensive for high-risk infants born prematurely or with very low birth weight, and can involve multiple specialists. The long-term goal is to identify any disabilities or delays early and provide intervention to prevent or reduce impairments.