This document discusses developmentally supportive care for preterm infants in the NICU. It aims to improve outcomes by supporting brain development, motor skills, sensory systems and family involvement through careful handling, positioning, feeding practices and control of the neonatal environment. Key aspects of care include protecting sleep, minimizing pain and stress, developmental activities like feeding and skin care, family centered care, and providing appropriate light, sound, and a caring staff. This holistic approach can help preterm infants heal and develop normally.
![Synactive theory
Focuses on the neurobehavioral capacity of the
infant as the baby develops
The baby’s neurobehavioral capacity develops
through interactions with caregivers and the
environment [i.e. sensory, medical, and care
giving experiences in the NICU]](https://image.slidesharecdn.com/developmentalsupportivecareinnicu-220203070007/85/Developmental-supportive-care-in-nicu-38-320.jpg)
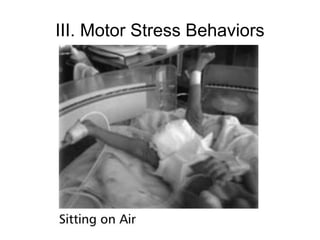
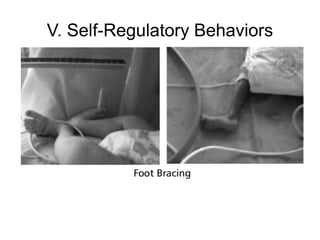
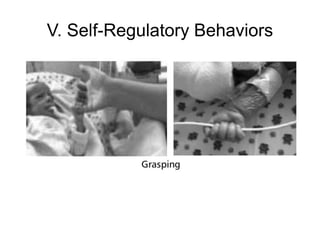
![[A] Assessment/observation of stress
Stress behaviors
I. Behavioral States (sleep states or states of
arousal)
II. Autonomic stress (signs) behaviors
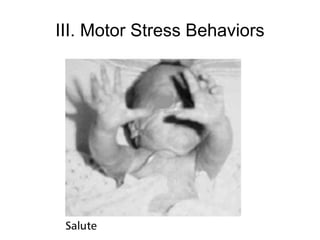
III. Motor Stress Behaviors
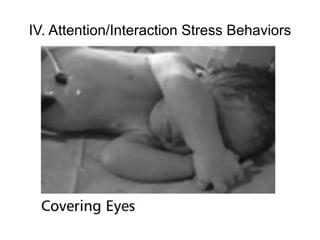
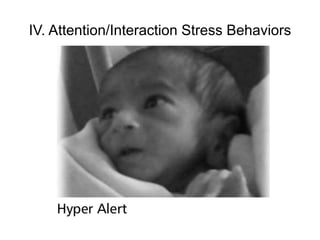
IV. Attention/Interaction Stress Behaviors
V. Self-Regulatory Behaviors](https://image.slidesharecdn.com/developmentalsupportivecareinnicu-220203070007/85/Developmental-supportive-care-in-nicu-42-320.jpg)

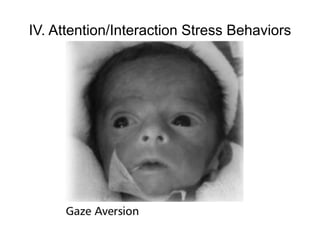
![2. Basic care and handling during
activities of daily living
Such as feeding, [nappy changes, bathing],
positioning and maintaining skin integrity
Greet with soft talk to the baby before touching, at
the onset to any handling or procedure.
Monitor baby’s response to soft talking during
routine care- when baby pays attention and does
not display stress, then this can be a good (brief)
time for this bonding or social interactive activity.
It is important to stop the interaction when the
baby demonstrates stress-gaze aversion or other.](https://image.slidesharecdn.com/developmentalsupportivecareinnicu-220203070007/85/Developmental-supportive-care-in-nicu-73-320.jpg)