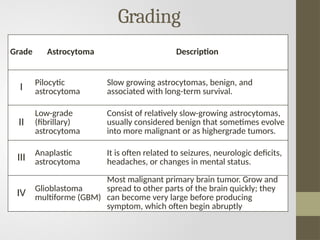
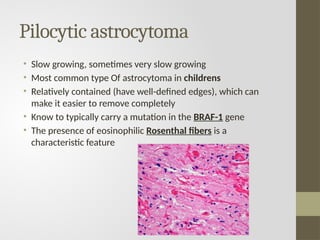
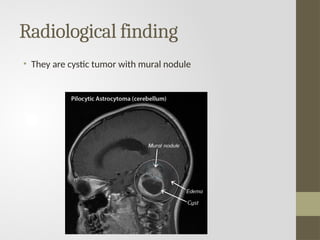
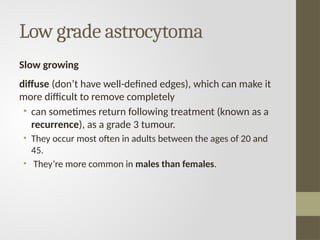
Astrocytomas are a common group of primary brain tumors originating from glial cells that support neurons, with various grades indicating different levels of malignancy. The most frequent types include pilocytic astrocytoma in children and glioblastoma multiforme in adults, which is the most aggressive and deadly form. Treatment approaches vary by tumor grade and may include surgery, radiotherapy, and chemotherapy, depending on individual cases.

![• Mostly it is supratentorial in adults: Cerebral cortex (MC
site)
• Mostly it is infratentorial in children: Cerebellum (MC
site)
• MC type of astrocytoma in children: Low grade-Pilocytic
astrocytoma (Best prognosis)
• MC type in adults; High grade Glioblastoma Multiforme
[GBM: most malignant (Worst prognosis)]](https://image.slidesharecdn.com/astrocytomappt-241126100903-1814fc0a/85/astrocytoma-ppt-pptx-5-320.jpg)