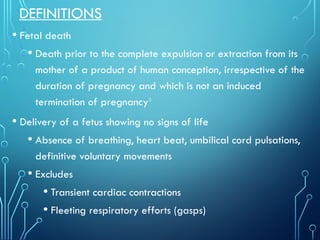
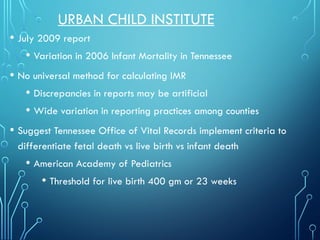
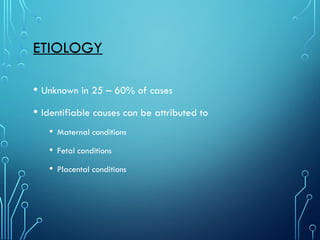
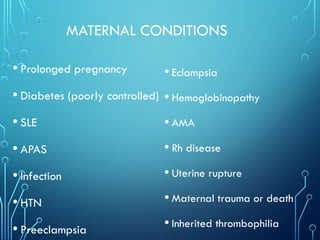
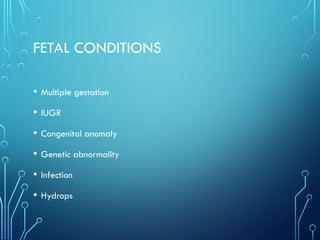
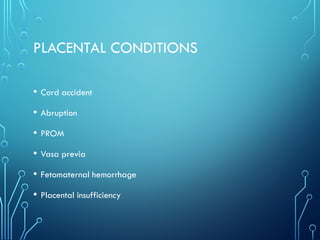
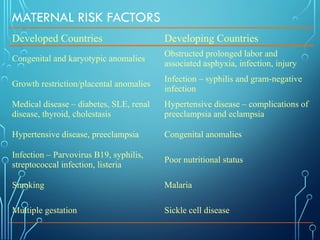
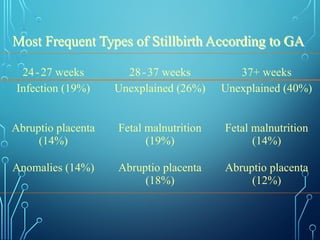
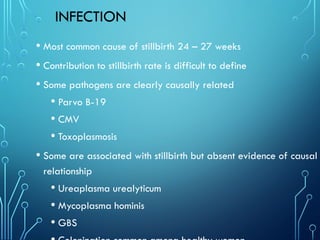
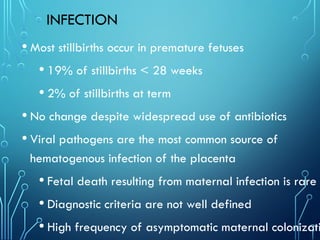
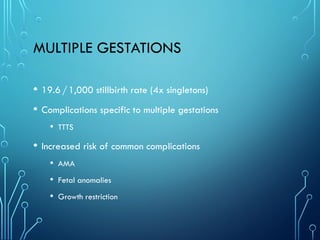
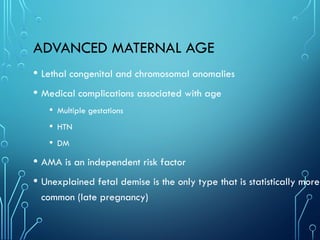
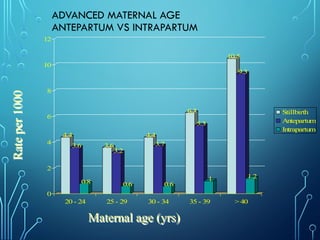
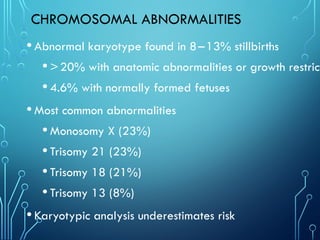
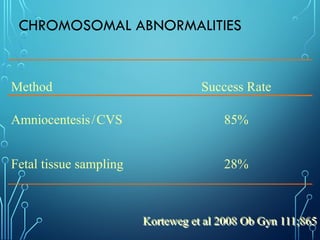
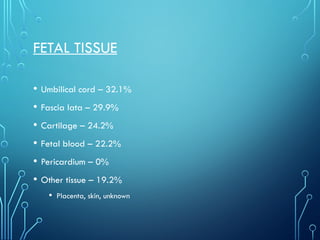
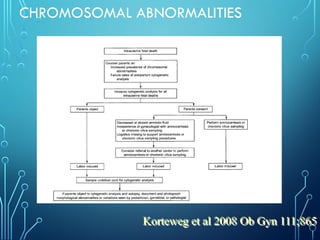
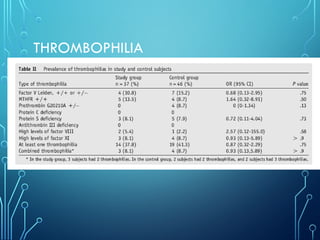
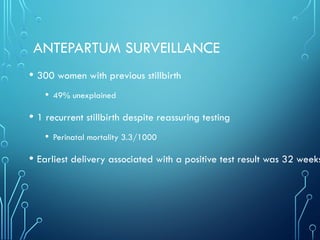
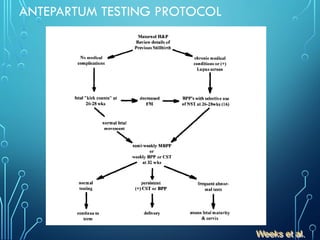
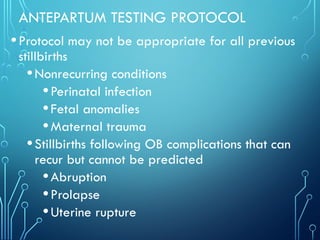
The document discusses stillbirth definitions, incidence, risk factors, and causes, noting that over 3 million stillbirths occur worldwide annually, with various maternal, fetal, and placental conditions involved. It highlights the disparities in stillbirth rates among different racial groups and the importance of gestational age in classifying stillbirths. Additionally, it outlines the complexities involved in antepartum surveillance and the limitations of existing screening methods for previous stillbirths.