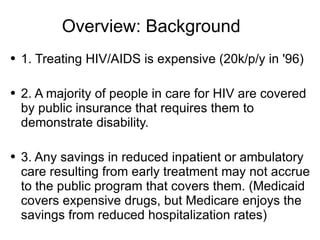
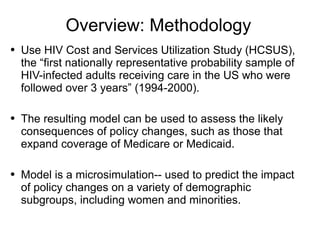
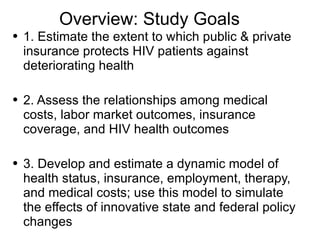
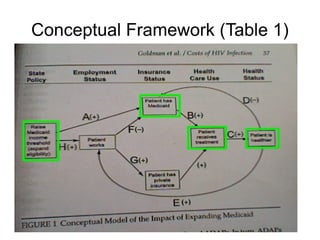
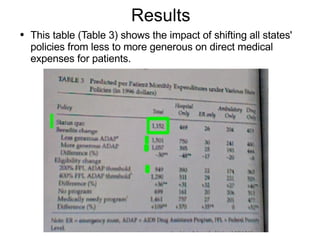
The document summarizes a study that used a microsimulation model to analyze the impacts of state policies on health outcomes and costs for people living with HIV/AIDS. The study used national data to estimate relationships between insurance coverage, health status, employment, treatment and medical costs. The model allowed researchers to simulate the effects of more generous state policies on economic outcomes. The researchers found that more generous policies, like increasing Medicaid eligibility, could improve health outcomes while increasing short-term costs for treatment but decreasing long-term hospitalization costs. However, the savings may not fully benefit the programs paying for increased treatment.