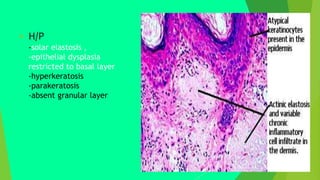
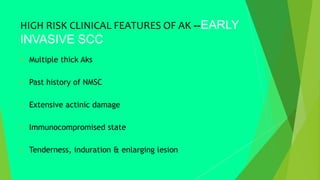
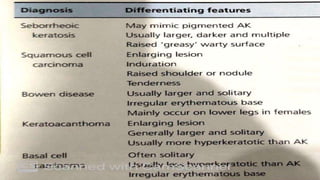
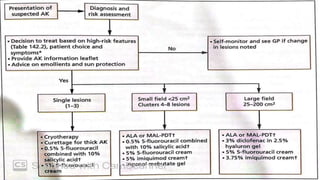
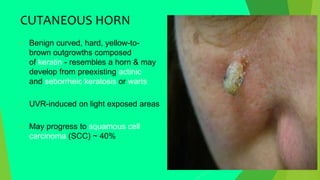
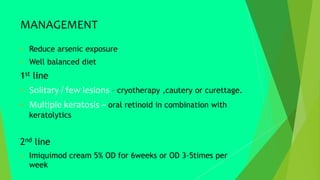
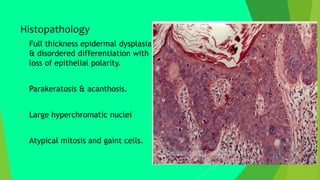
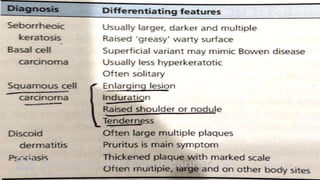
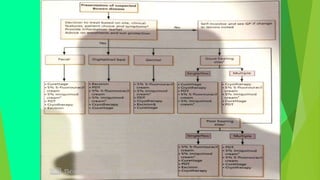
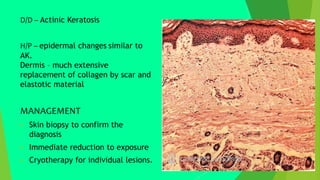
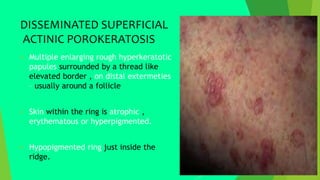
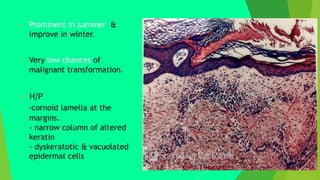
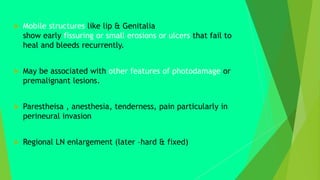
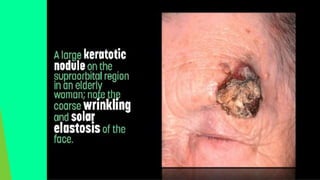
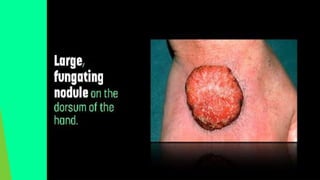
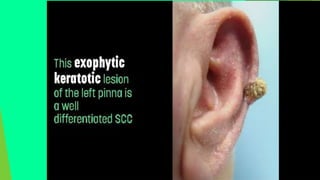
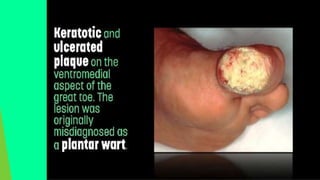
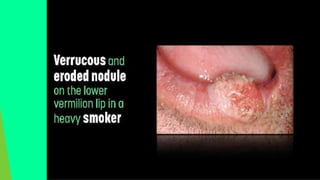
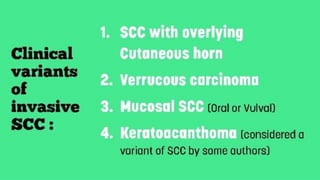
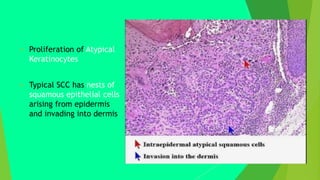
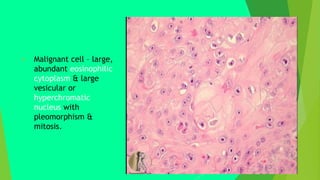
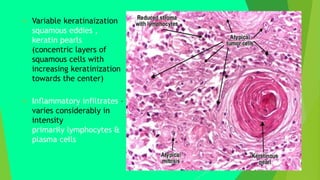
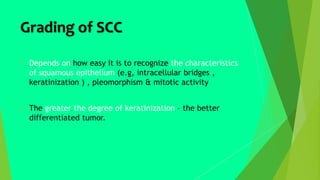
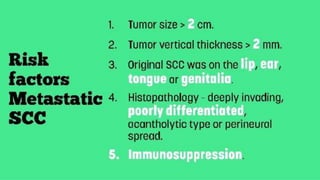
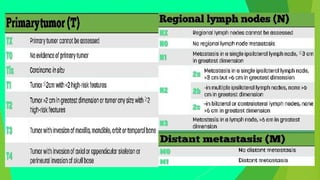
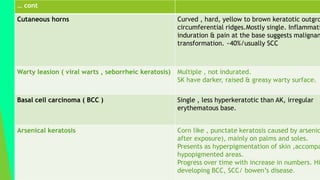
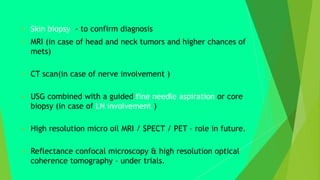
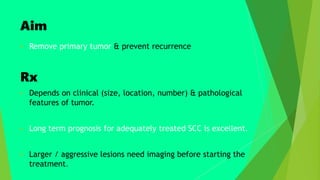
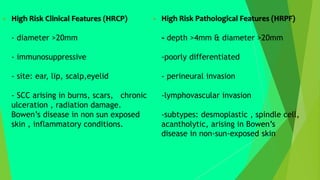
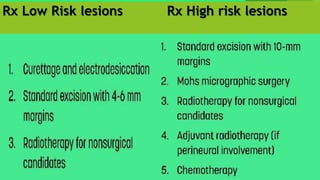
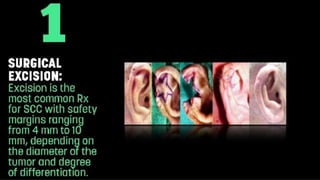
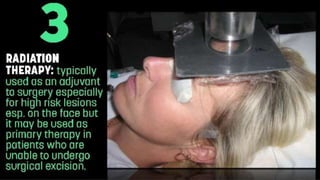
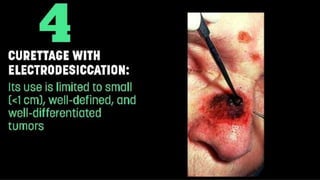
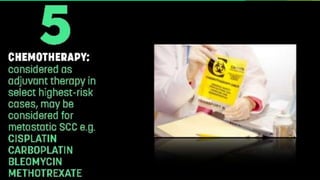
The document discusses various types of squamous cell carcinoma (SCC) and their precursor lesions, including actinic keratosis, cutaneous horn, arsenical keratosis, and Bowen's disease. It provides details on their clinical features, risk factors, potential for malignant transformation, and management options. The document emphasizes the importance of early diagnosis and treatment, as well as the differing risks associated with various clinical presentations.