This document discusses several conditions related to the skin:
1. Miliaria is caused by blocked sweat ducts, presenting as clear, red, or deeper colored bumps depending on the depth of blockage. Treatment focuses on keeping cool and dry.
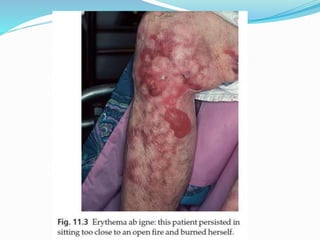
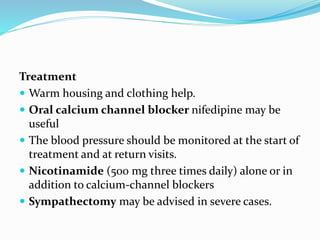
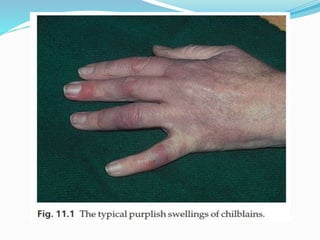
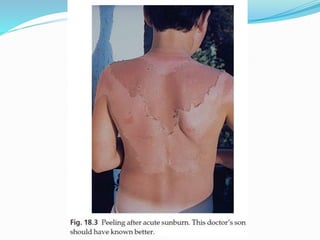
2. Erythema ab igne, perniosis, Raynaud's phenomenon, and sunburn are all conditions caused by exposure to heat or cold and present with redness, swelling, or discoloration of the skin. Management prioritizes avoidance of triggers and medication for symptoms.
3. Callosities and corns develop from pressure and friction, with corns specifically causing pain. Treatment aims to reduce pressure through padding or