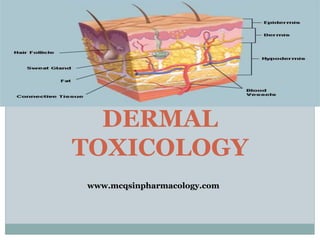
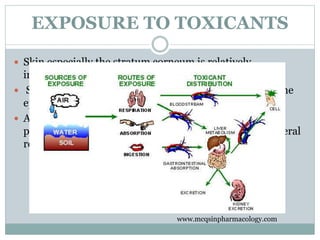
The document provides an overview of dermal toxicology, detailing the structure and functions of skin layers, the metabolism of xenobiotics, and the effects of toxicants on skin health. It discusses various skin conditions caused by exposure to toxic substances, including allergic reactions, photosensitization, hyperkeratosis, and different types of skin cancer. Management strategies and preventive measures for skin-related toxicities are also outlined.