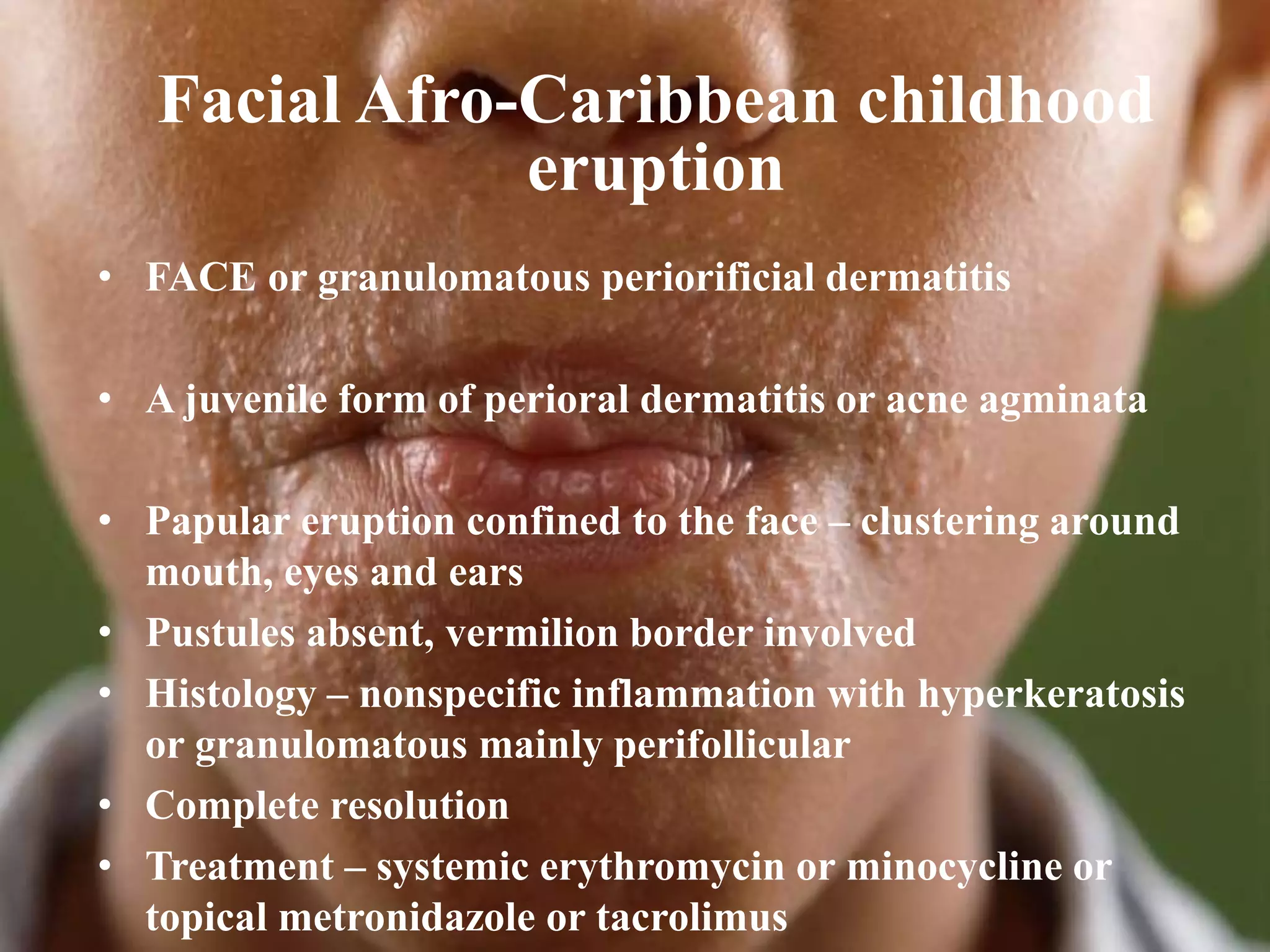
This document provides a classification and overview of the differential diagnosis of papular lesions that can occur on the face. It categorizes potential causes into infections, inflammatory disorders, tumors, and others. Key points include descriptions of common infections like molluscum contagiosum and lupus vulgaris. Inflammatory conditions discussed are acne, rosacea, perioral dermatitis, and sarcoidosis. Benign and malignant tumors of the skin and adnexal structures are also reviewed. Differential diagnoses and treatment approaches are mentioned for many of the conditions.