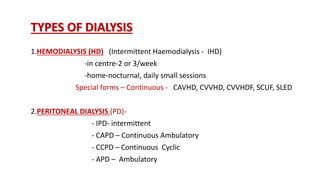
This document discusses management of end-stage renal disease (ESRD) through dialysis and transplantation. It describes the main types of dialysis as hemodialysis and peritoneal dialysis. Hemodialysis is the most common method and involves purifying the blood through diffusion and ultrafiltration. Peritoneal dialysis uses the peritoneal membrane in the abdominal cavity for diffusion and ultrafiltration. Kidney transplantation is also discussed as the best treatment for ESRD when a donor organ is available. The document outlines donor sources, compatibility testing, transplantation procedure, and potential complications.