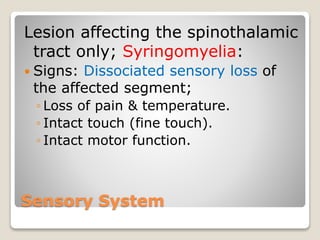
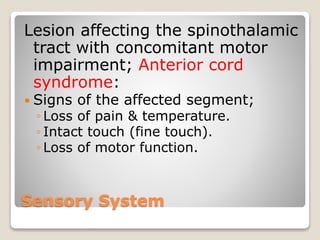
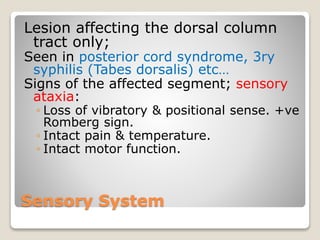
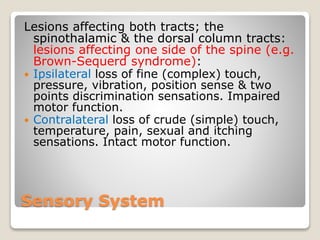
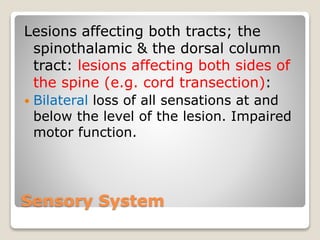
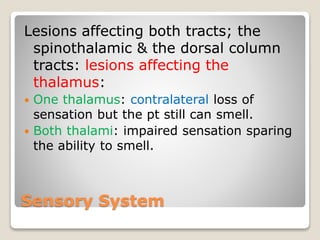
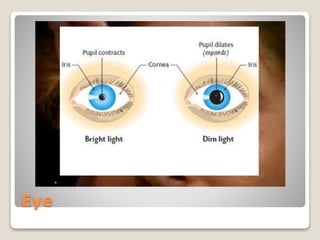
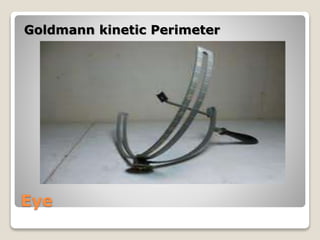
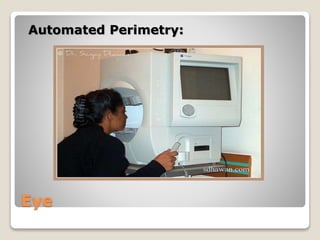
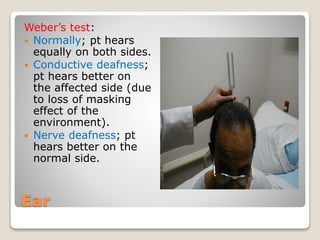
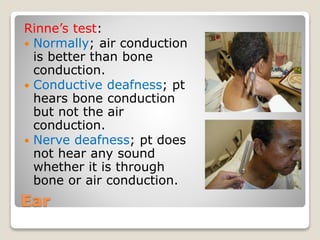
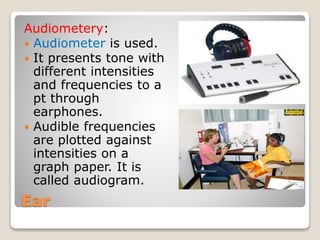
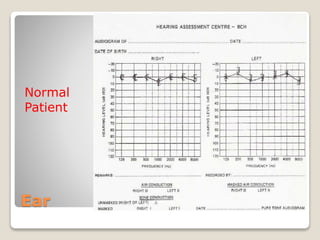
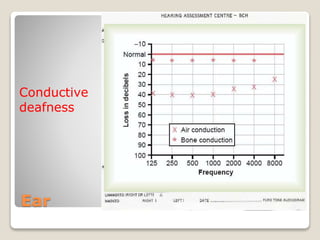
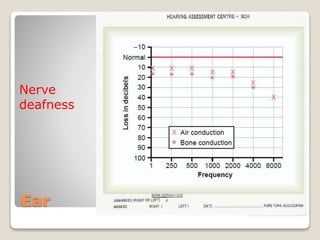
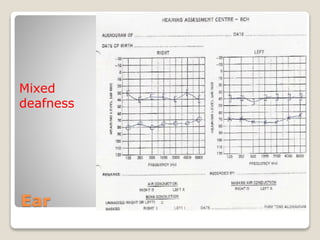
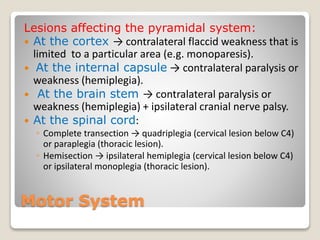
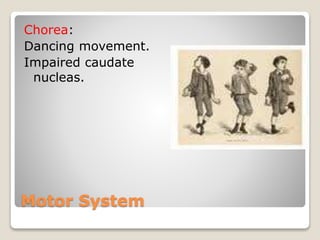
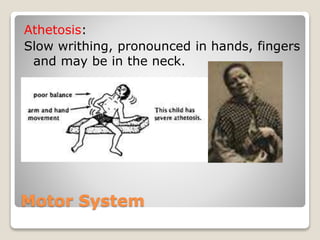
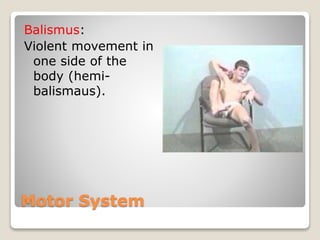
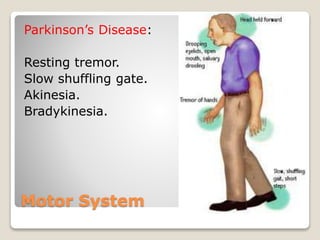
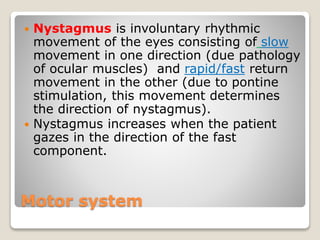
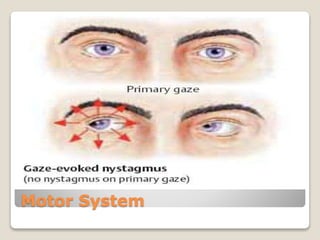
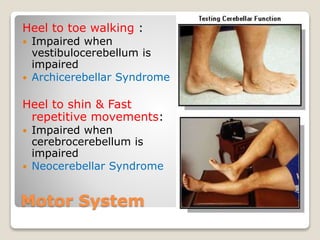
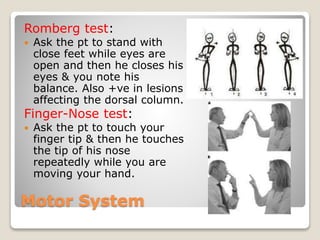
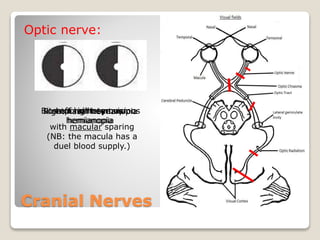
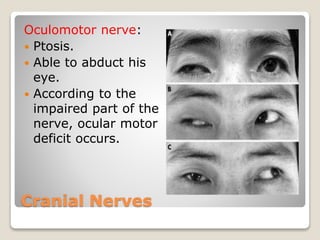
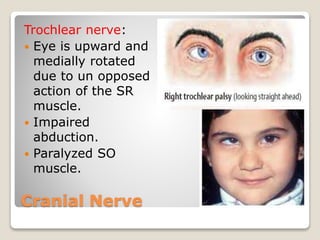
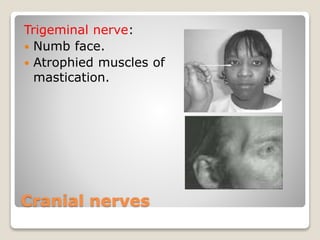
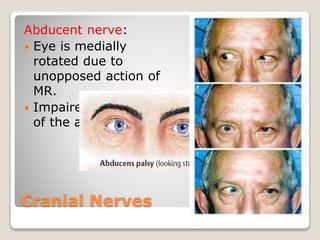
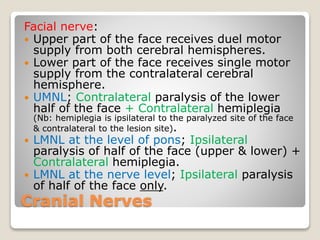
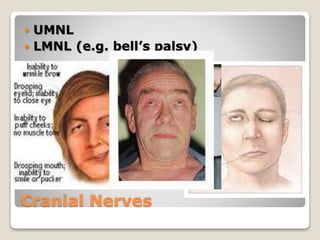
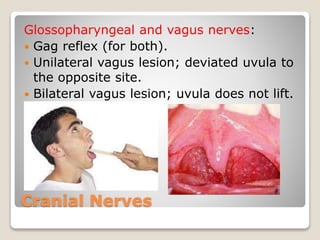
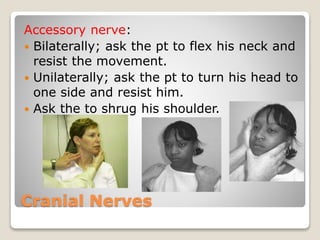
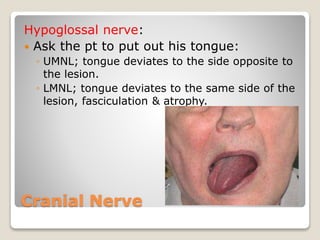
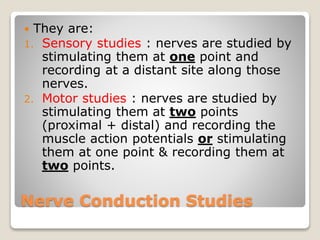
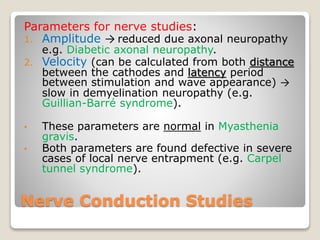
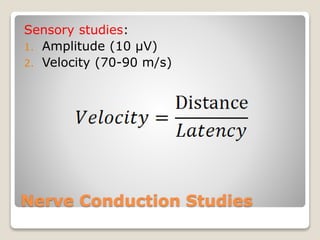
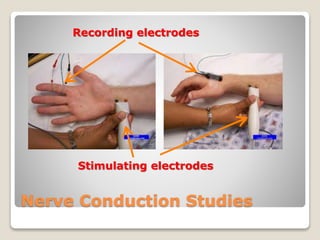
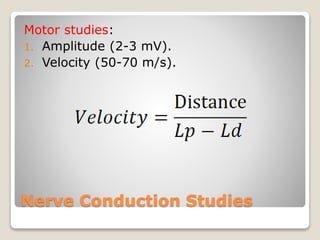
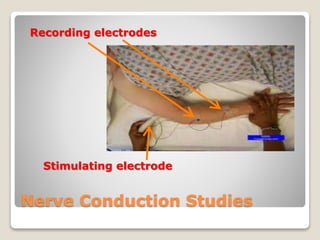
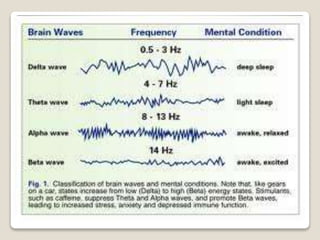
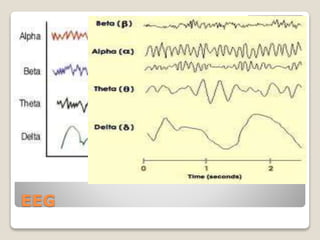
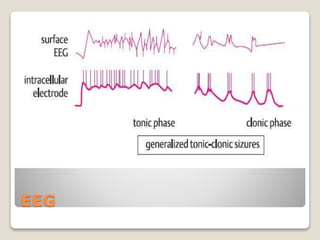
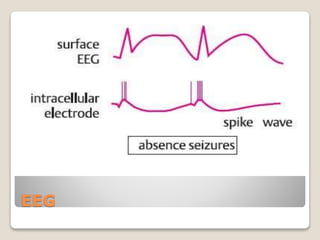
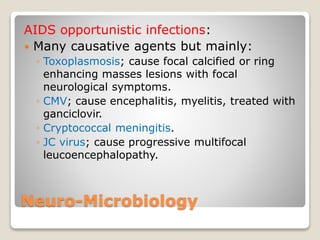
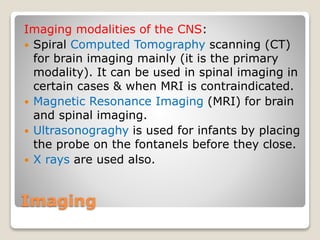
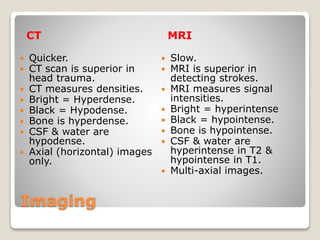
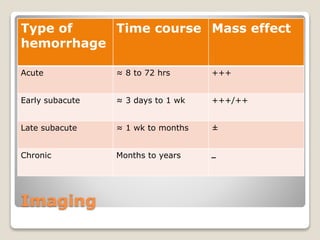
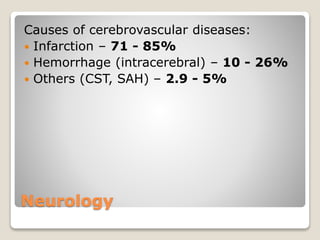
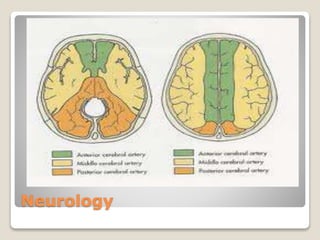
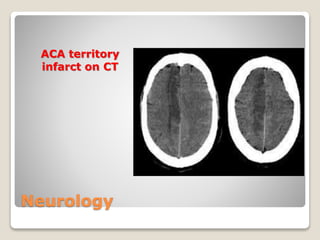
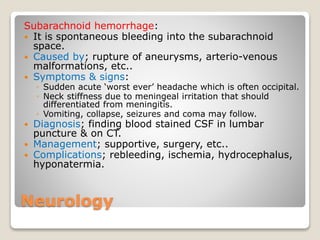
This document provides an overview of topics in applied neurosciences. It discusses the sensory system, special senses including the eye and ear, the motor system, cranial nerves, nerve conduction studies, EEG, neuro-microbiology, and several neurological disorders. Specific signs and symptoms of lesions in different areas of the nervous system are described. Various examination techniques for assessing the sensory and motor systems are also outlined.