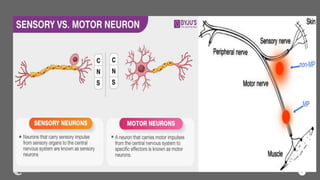
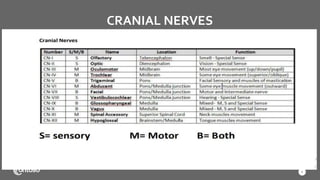
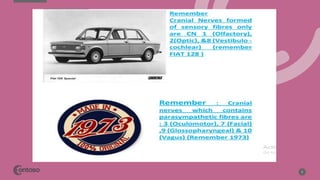
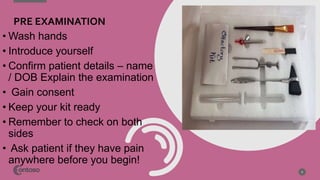
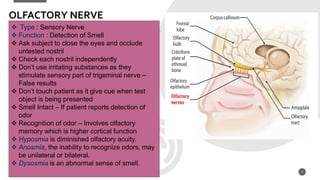
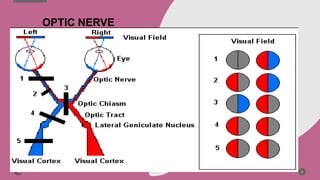
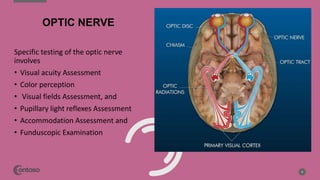
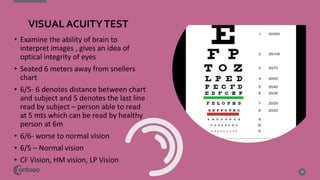
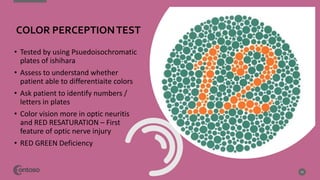
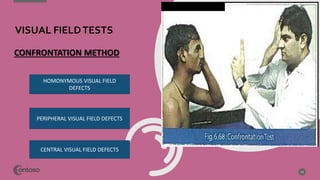
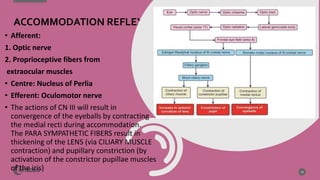
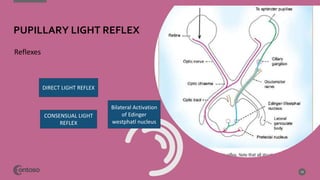
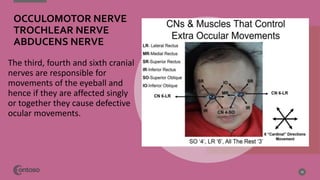
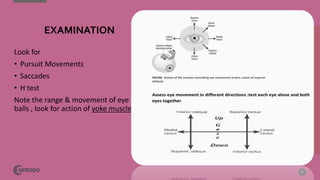
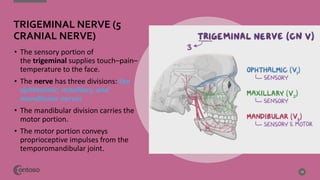
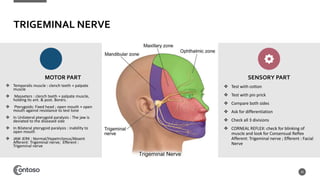
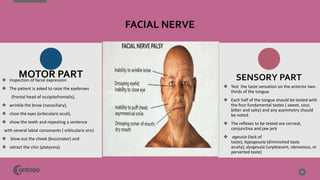
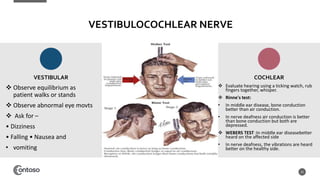
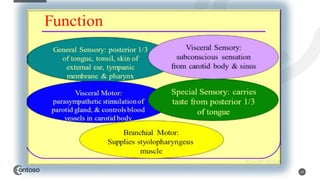
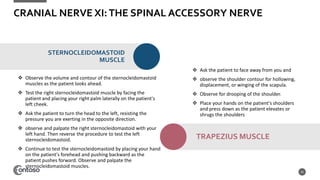
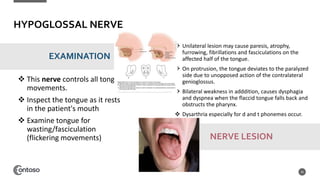
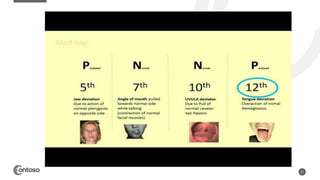
This document provides guidance on performing a cranial nerve examination. It discusses the 12 cranial nerves and how to test each one. For each nerve, it describes the nerve's function, testing procedures, what abnormalities indicate a lesion, and other relevant clinical information. The examination procedures are described in detail, including how to test visual acuity, visual fields, pupillary reflexes, hearing, facial expression, tongue movement, and more. References are provided for additional information.