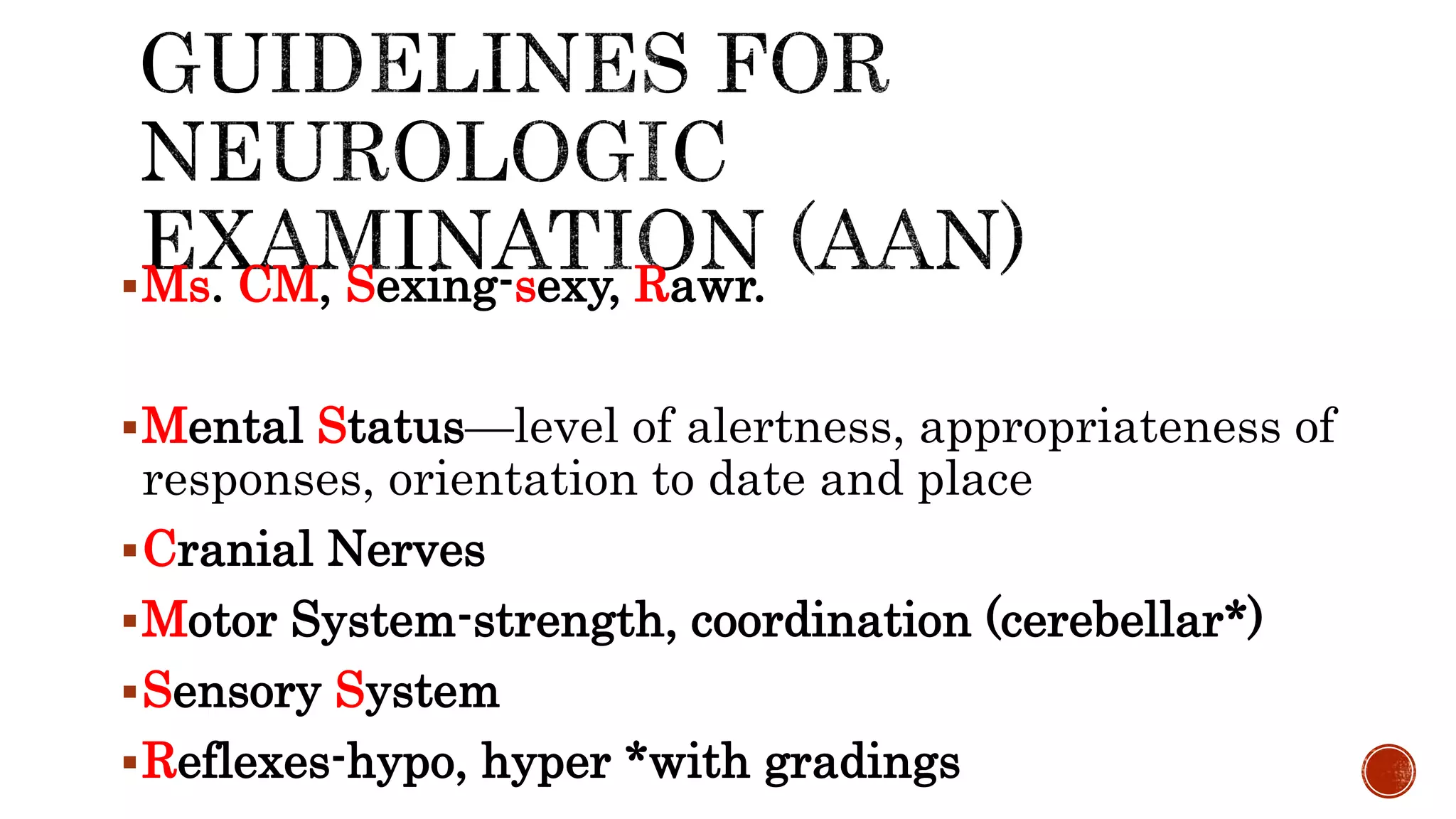
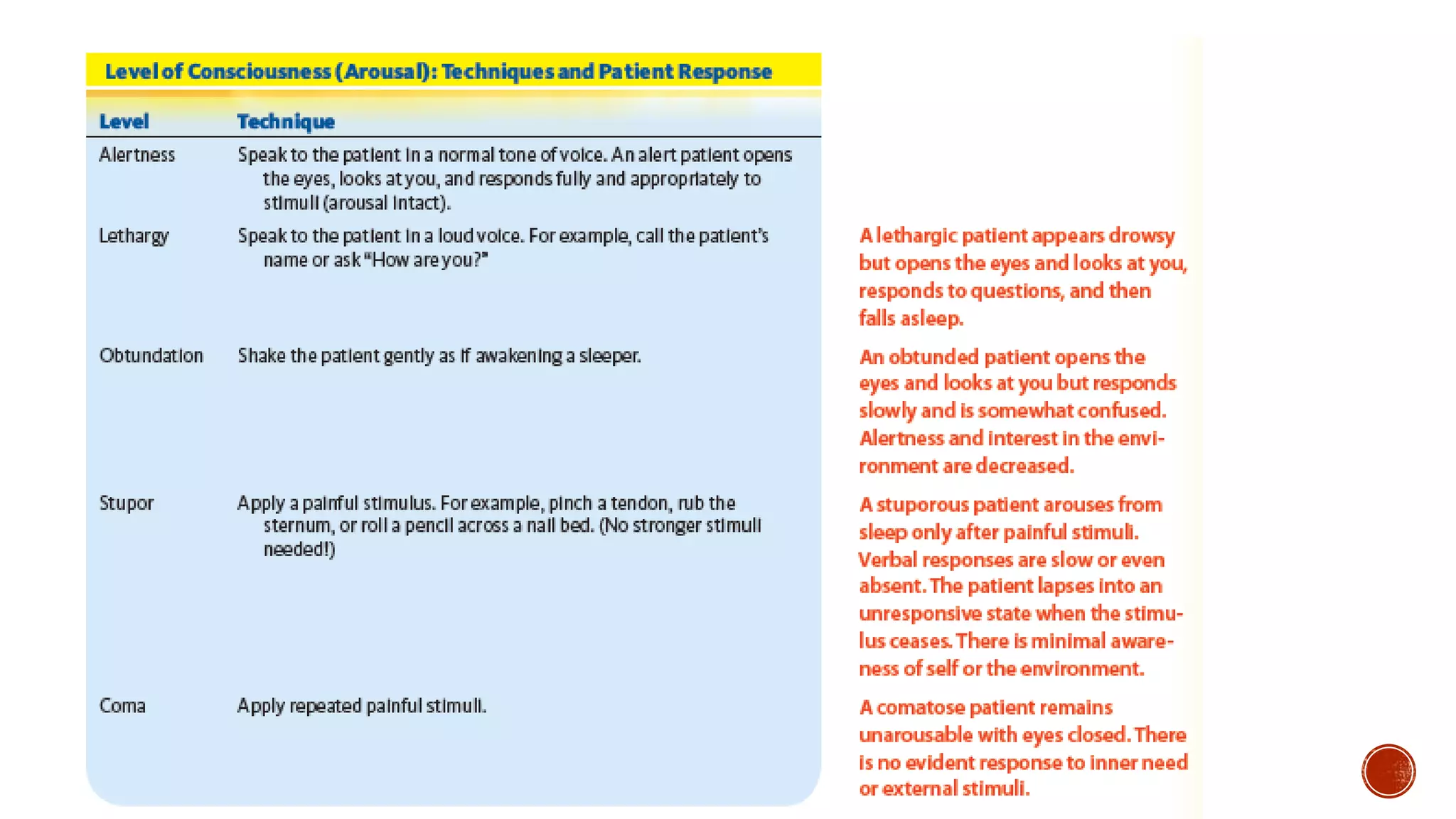
This document provides information about Baymax, who introduces himself as a personal healthcare provider. It then provides details on performing a physical exam, including preparing for the exam, establishing rapport with the patient, ensuring privacy and comfort, and explaining findings. Common symptoms that may warrant examination are listed. The physical exam components covered include vital signs, skin, head, eyes, ears, nose, mouth, neck, lungs, heart, abdomen, back, extremities, neurologic exam and mental status exam.