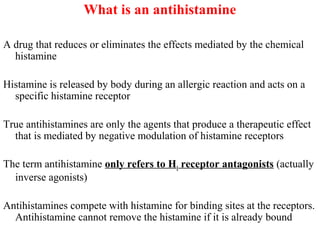
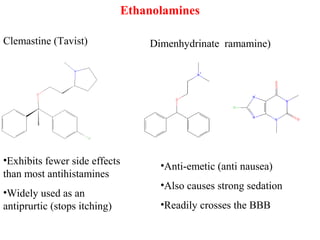
This document provides an overview of antihistamines and allergies. It defines antihistamines as drugs that reduce the effects of histamine, which is released during allergic reactions. The document discusses the causes of allergies and the role of histamine. It also outlines the different classes of antihistamines, including first generation antihistamines and their associated side effects, as well as newer second generation antihistamines that are more selective. The clinical uses of antihistamines and future directions for allergy treatment are also briefly mentioned.