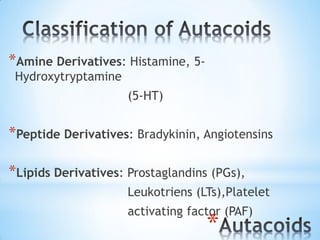
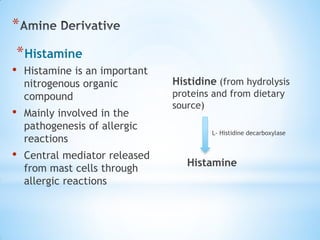
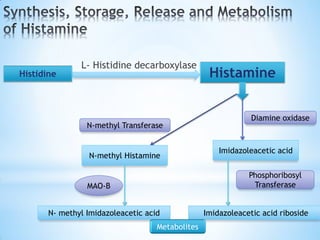
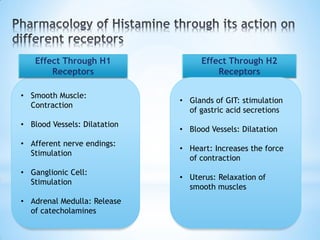
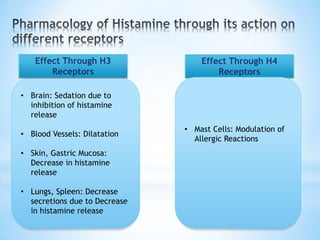
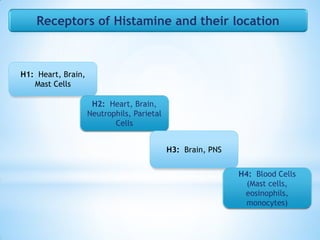
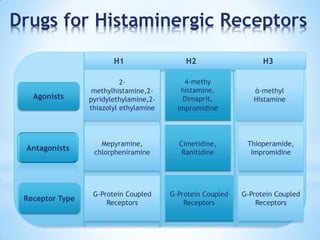
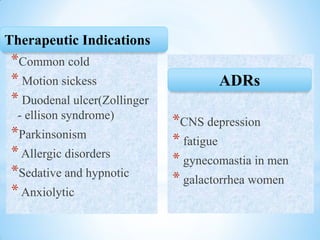
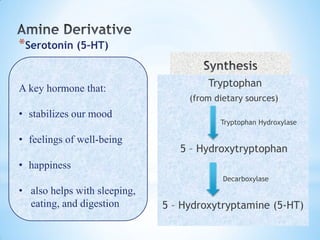
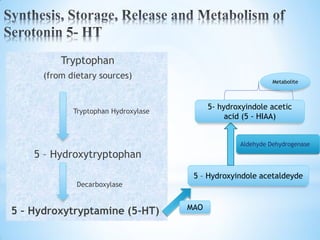
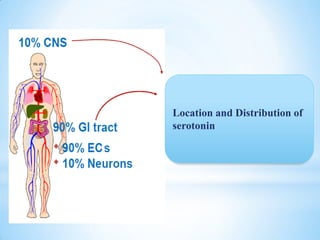
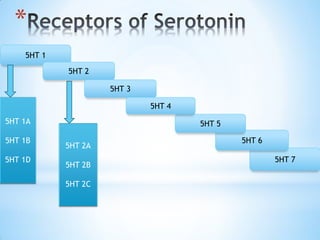
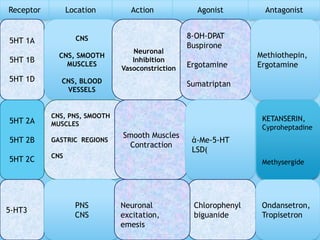
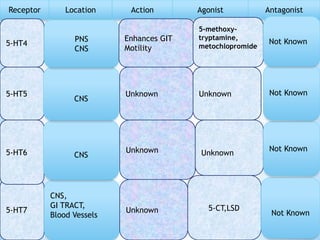
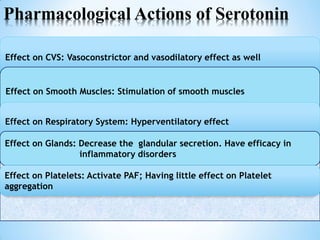
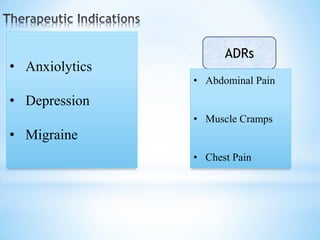
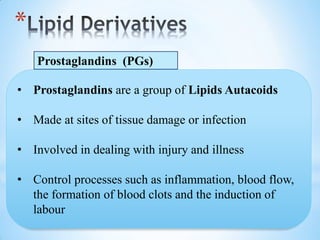
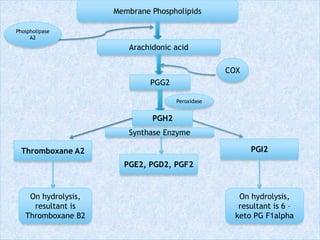
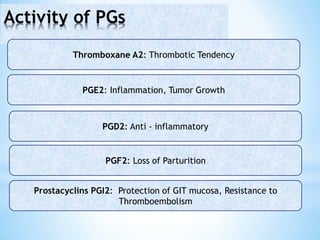
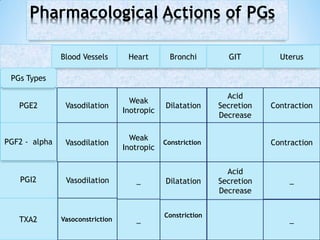
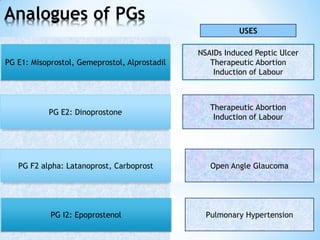
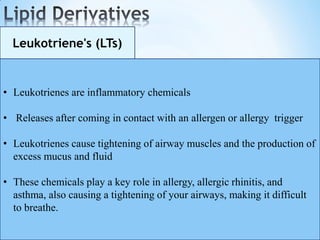
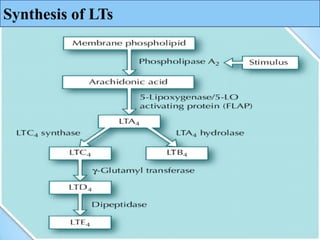
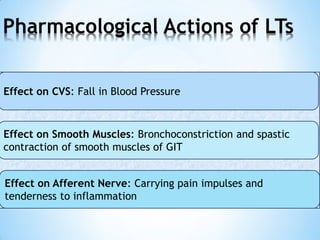
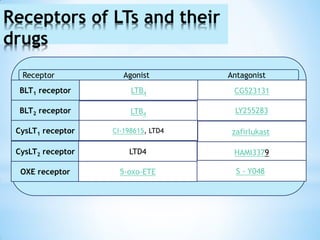
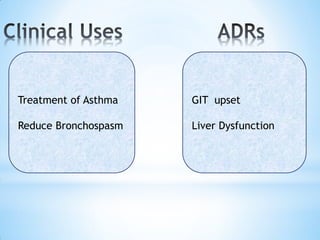
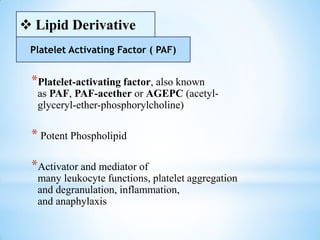
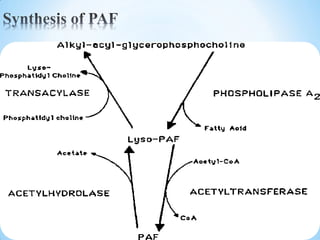
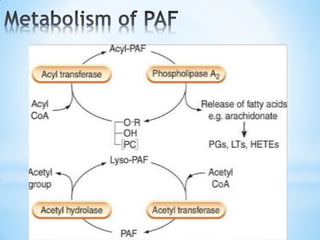
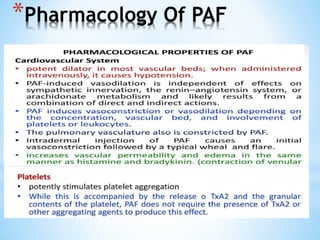
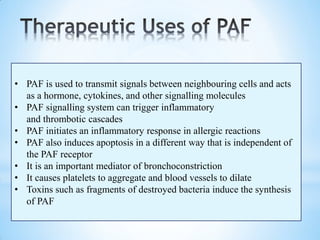
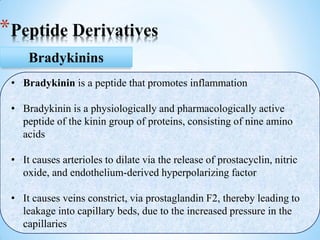
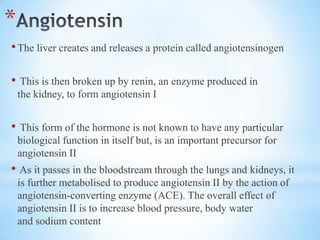
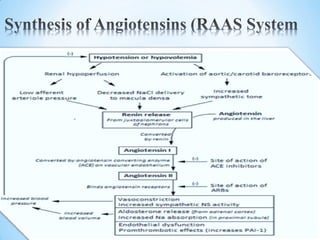
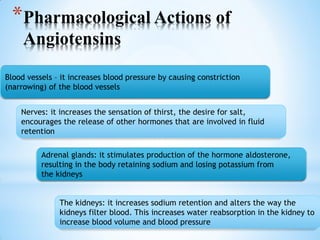
Local hormones, also known as autacoids, are physiologically active substances produced locally in the body that have short-lived, localized effects. Some key classes of local hormones include amine derivatives like histamine and serotonin, peptide derivatives like bradykinin and angiotensins, and lipid derivatives like prostaglandins, leukotrienes, and platelet activating factor. These endogenous compounds play important roles in physiological and pathological processes through their actions on local tissues.