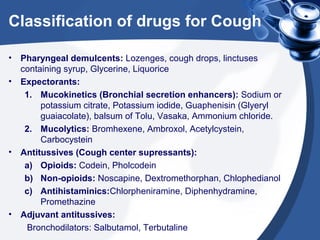
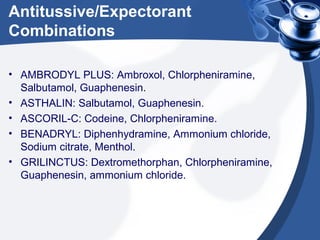
This document discusses drugs for cough. It begins by describing the mechanism and causes of cough. Cough can be voluntary or reflexive, and has afferent and efferent pathways involving various nerves. Causes include upper respiratory infections, pneumonia, and other conditions. The document then classifies drugs for cough into four main categories: pharyngeal demulcents to soothe the throat; expectorants to increase or thin mucus; antitussives to suppress coughing; and bronchodilators to relieve cough caused by bronchospasm. Specific drugs and combinations are provided as examples for each category. The document concludes by describing specific treatments for cough based on its underlying cause.