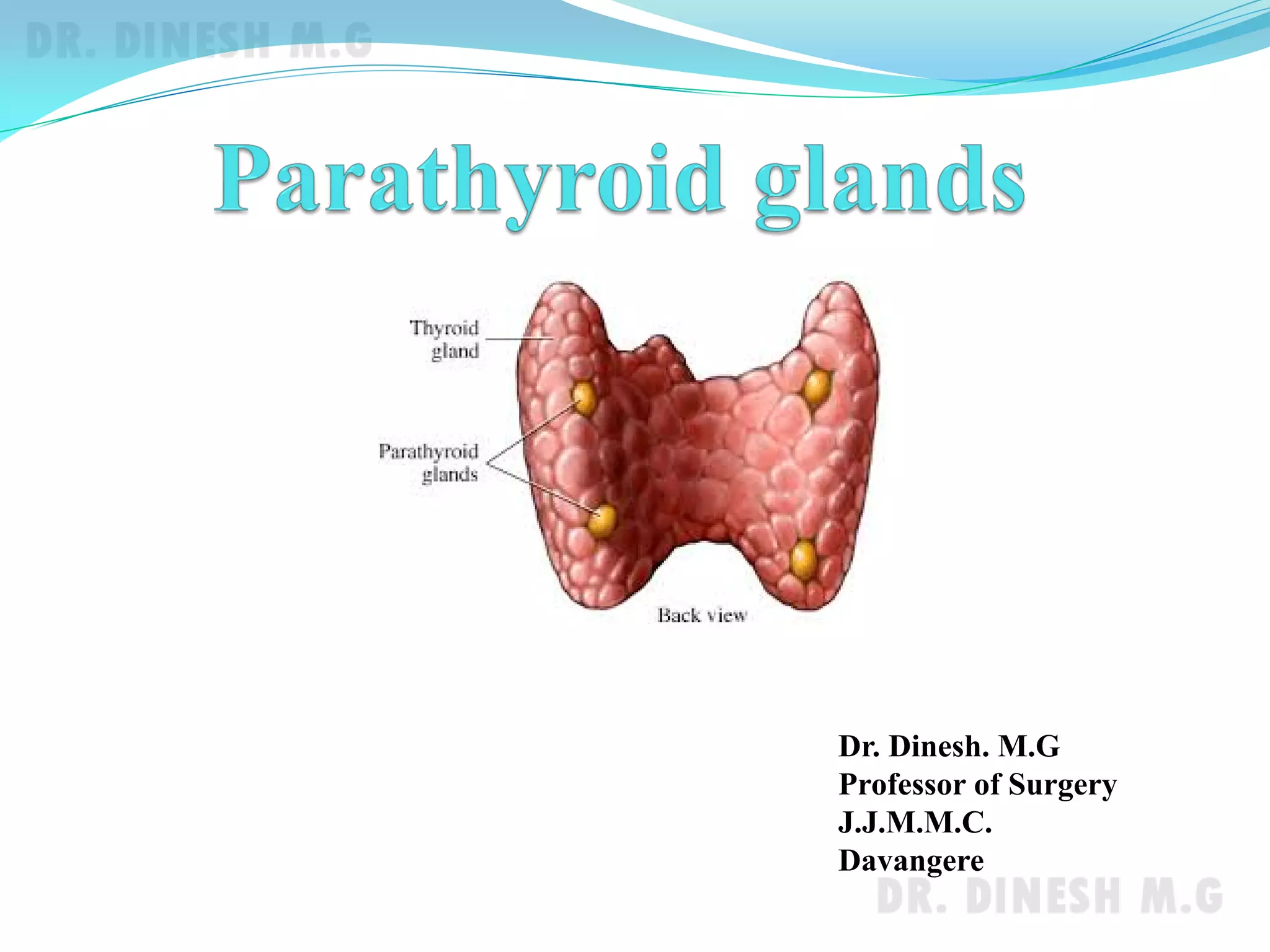
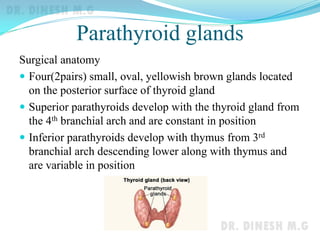
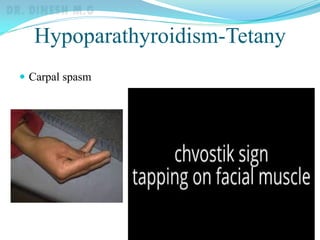
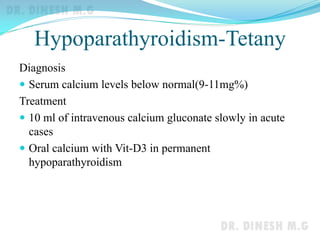
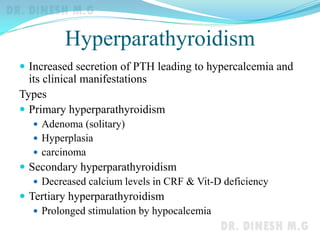
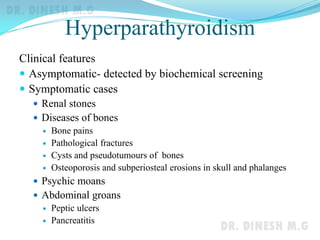
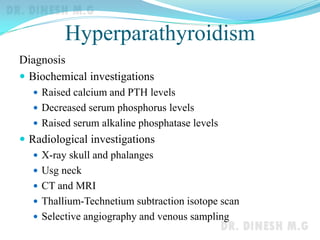
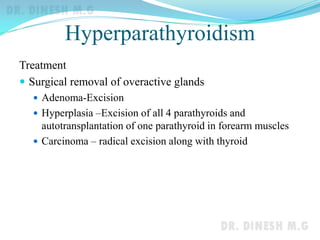
The document discusses the anatomy, physiology, and pathologies of the parathyroid glands. It describes the parathyroid glands as four small oval glands located on the posterior surface of the thyroid gland. The glands secrete parathyroid hormone (PTH) which regulates calcium levels. Hypoparathyroidism occurs when PTH levels are low, causing hypocalcemia and tetany. Hyperparathyroidism is caused by excessive PTH secretion leading to hypercalcemia. Surgical removal of overactive glands is used to treat hyperparathyroidism.