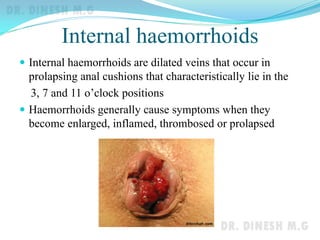
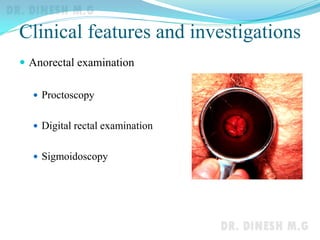
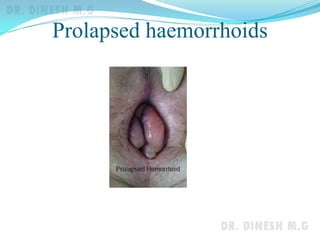
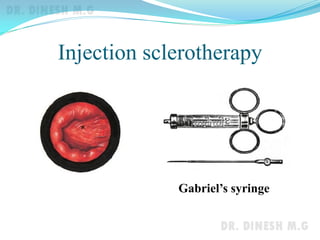
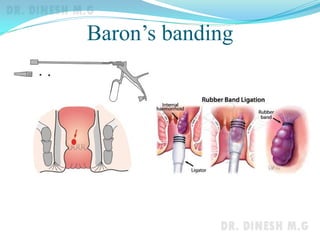
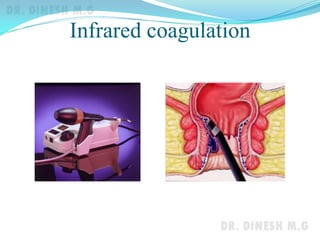
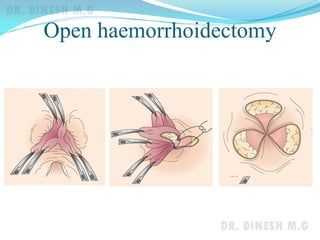
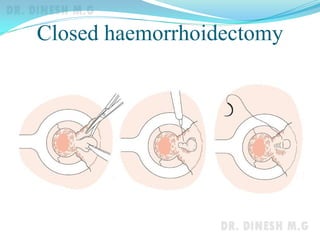
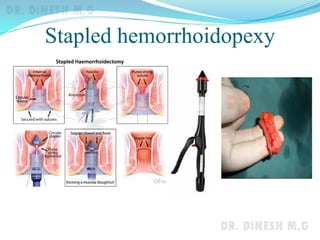
This document discusses the various causes of rectal bleeding, focusing on hemorrhoids. It defines internal and external hemorrhoids, explaining their locations and causes. Symptoms of internal hemorrhoids include painless bleeding during defecation and possible prolapse. Complications can include strangulation, thrombosis, and gangrene. Treatment options are discussed, including non-operative approaches like injection sclerotherapy, banding, and infrared coagulation, as well as operative techniques like open or closed hemorrhoidectomy and stapled hemorrhoidopexy. External hemorrhoids and related conditions are also briefly mentioned.