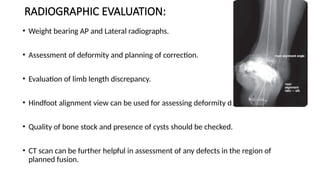
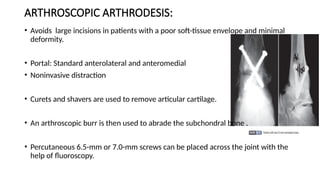
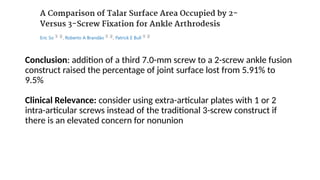
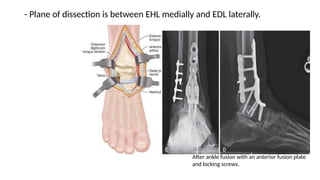
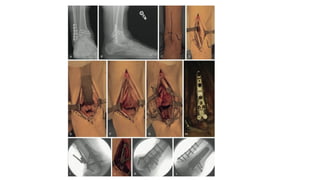
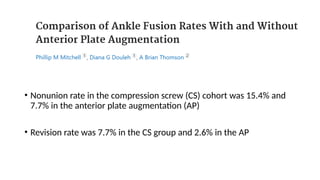
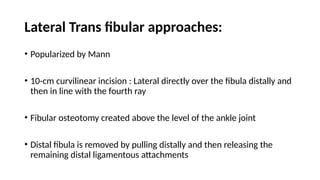
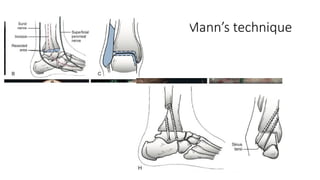
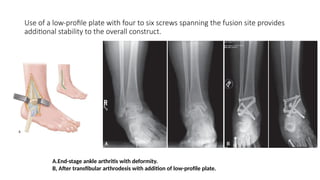
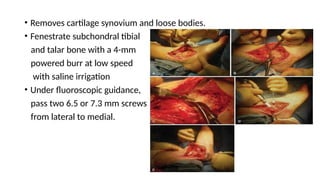
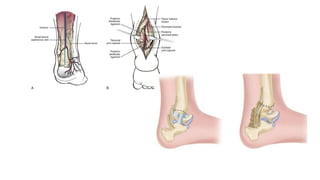
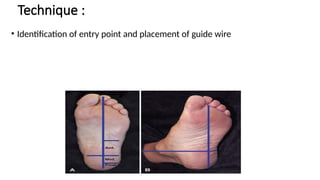
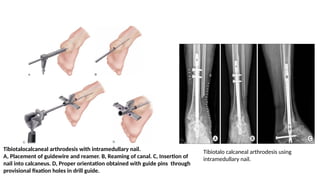
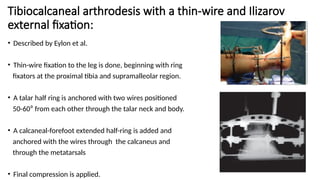
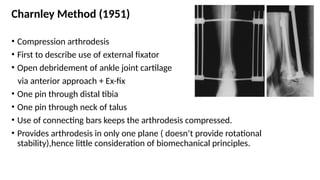
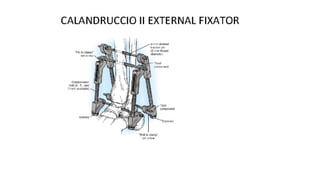
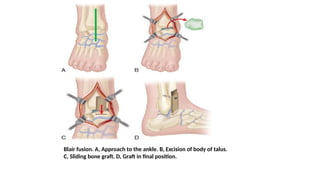
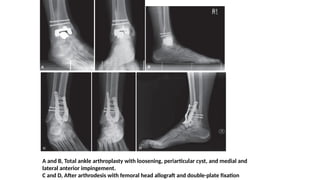
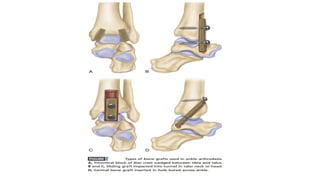
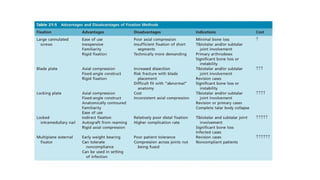
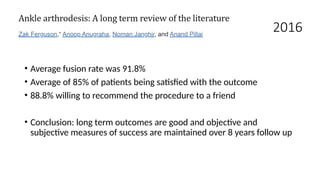
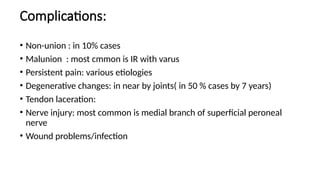
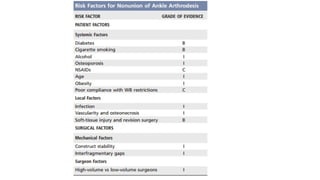
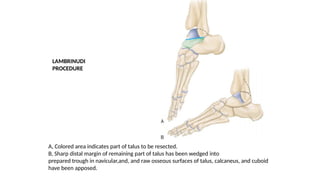
Ankle arthrodesis is a surgical procedure aimed at achieving irreversible fusion of the ankle joint to restore functionality and stability, particularly in cases of severe arthritis or instability. Techniques range from arthroscopic methods to mini-incision approaches, each with specific indications, advantages, and surgical principles, including proper alignment and bone graft usage. Complications can include non-union and degenerative changes in adjacent joints, with successful outcomes being reported in various studies.