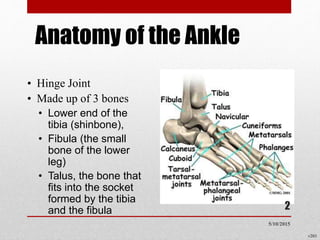
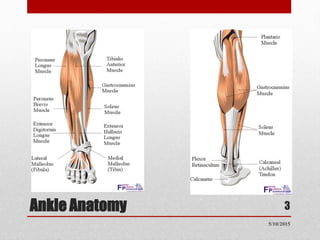
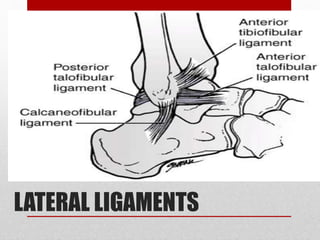
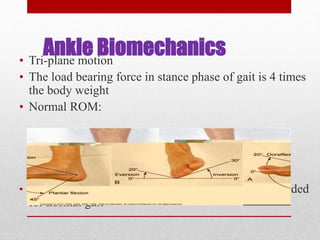
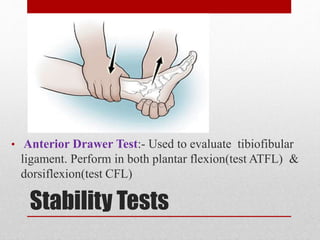
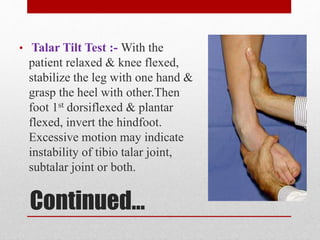
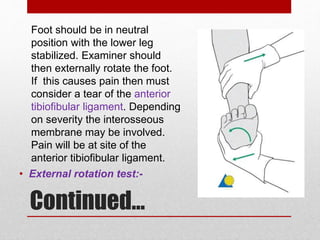
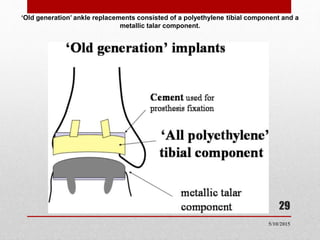
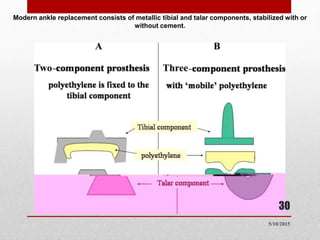
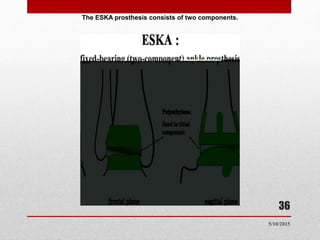
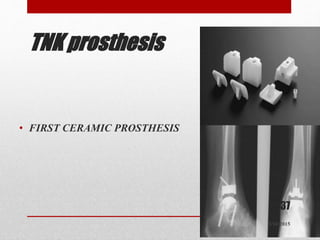
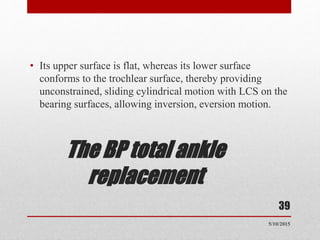
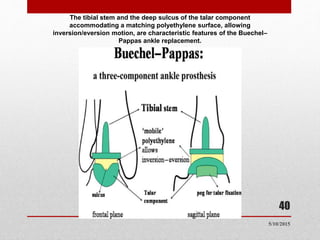
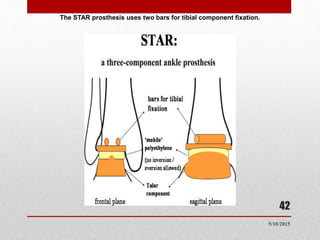
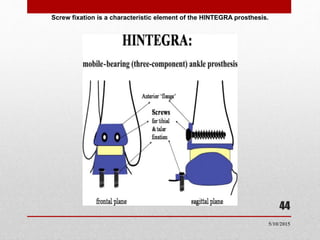
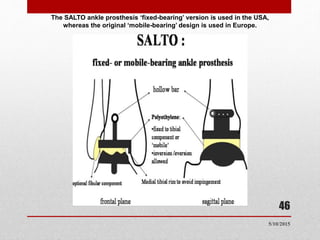
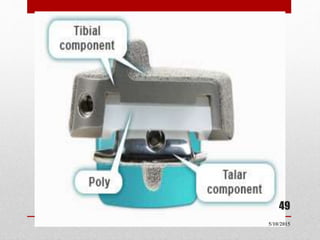
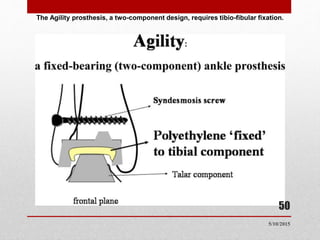
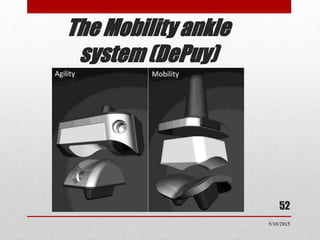
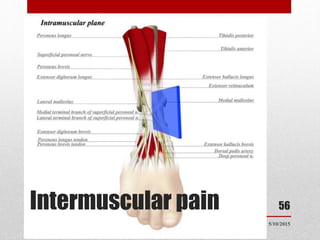
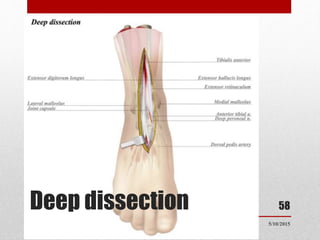
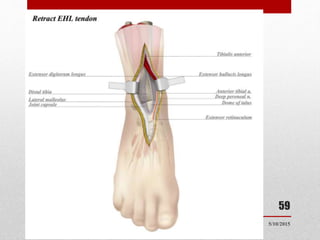
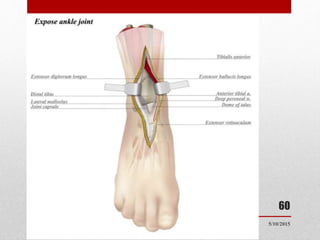
This document discusses total ankle replacement (TAR). It begins with the anatomy of the ankle joint and causes of ankle arthritis. Symptoms of ankle arthritis are described. The physical exam and tests to assess ankle stability are outlined. Treatment options for ankle arthritis include nonsurgical methods as well as different types of surgical procedures like arthrodesis (ankle fusion) and TAR. The history of TAR is summarized, including early constrained and unconstrained designs that had high failure rates. Modern TAR designs are classified and various implant systems currently in use are described, including their characteristics. The surgical approach and postoperative protocol for TAR are also summarized.