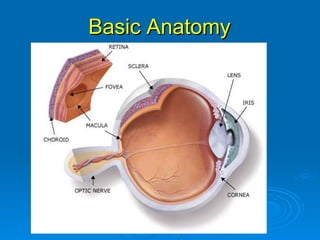
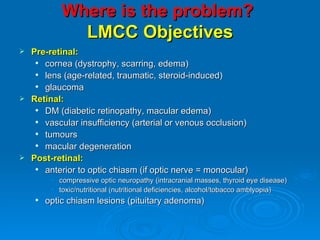
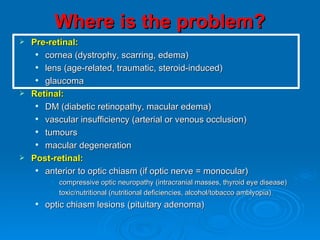
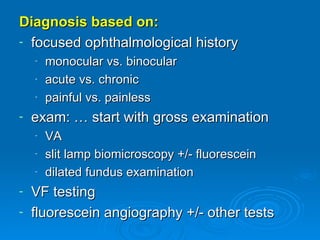
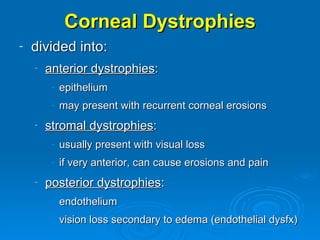
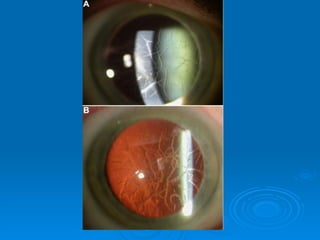
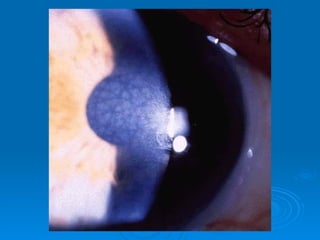
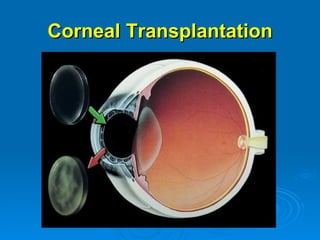
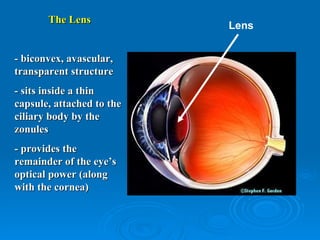
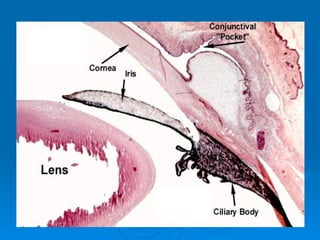
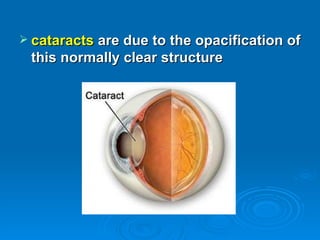
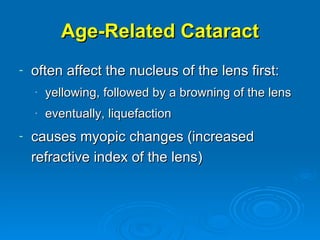
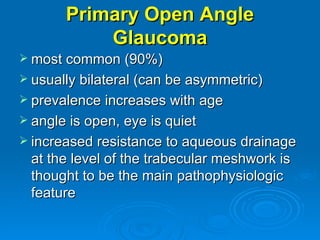
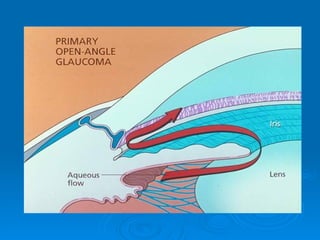
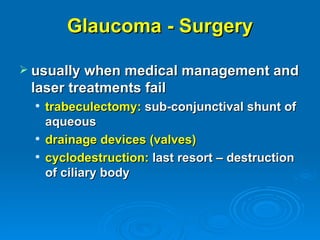
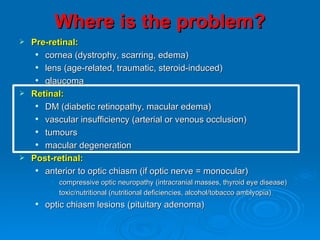
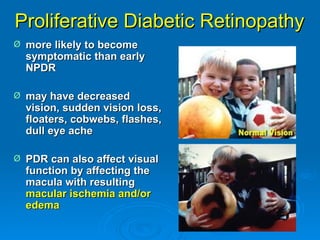
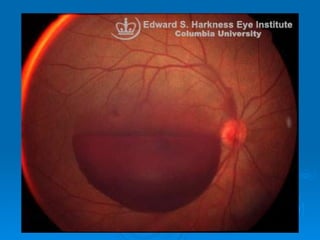
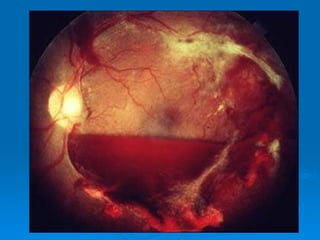
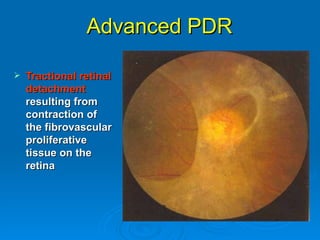
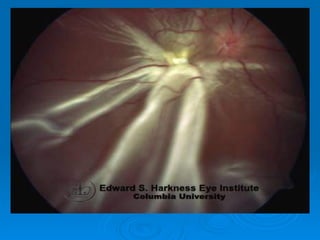
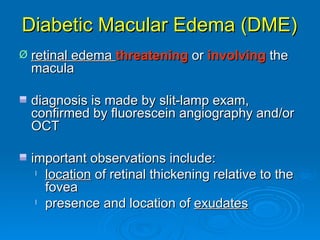
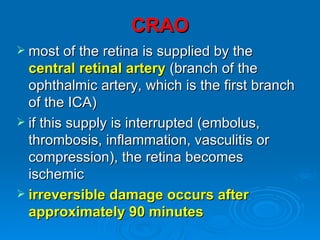
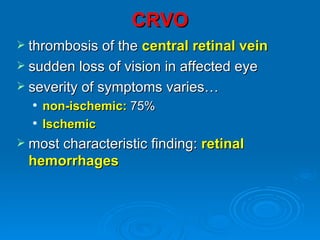
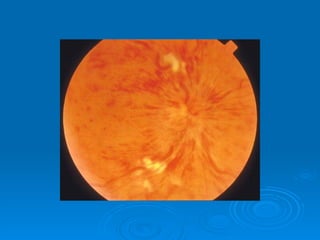
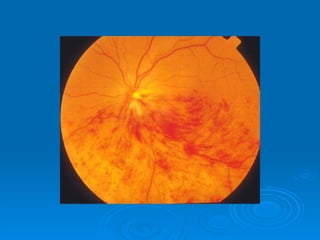
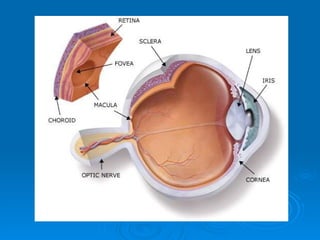
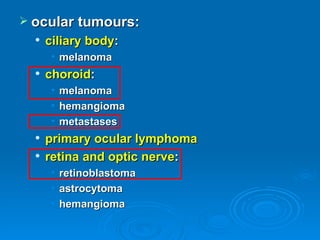
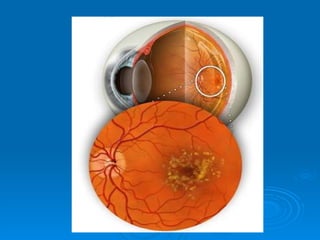
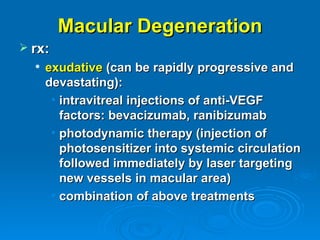
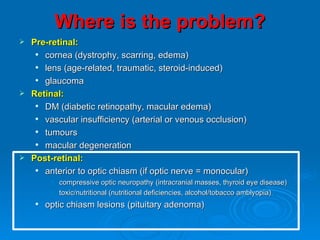
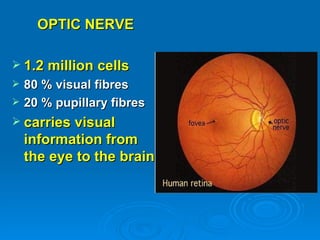
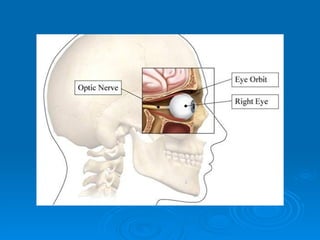
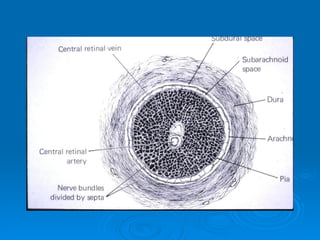
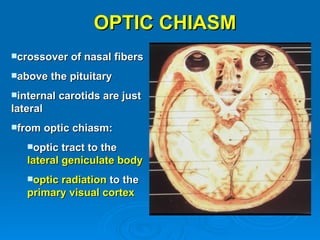
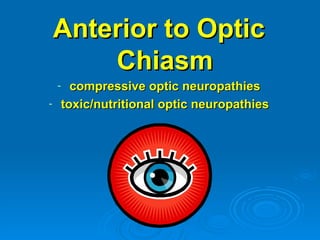
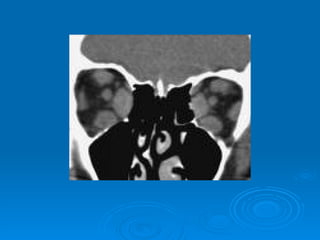
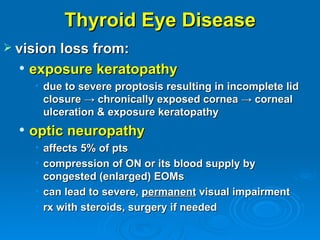
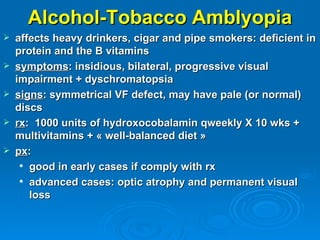
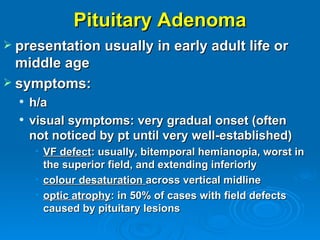
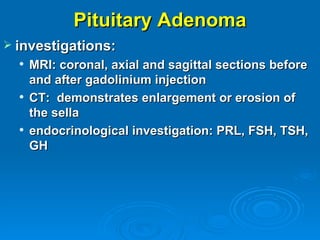
Chronic visual disturbance and loss can result from problems in three locations: pre-retinal, retinal, and post-retinal. Common pre-retinal causes include corneal dystrophy, scarring, or edema and lens issues such as cataracts. Retinal problems include diabetic retinopathy and macular edema, vascular occlusions, tumors, and macular degeneration. Post-retinal causes involve the optic nerve, such as glaucoma, compressive optic neuropathies, and nutritional deficiencies. A thorough exam and testing is needed to determine the specific location and cause of visual issues.