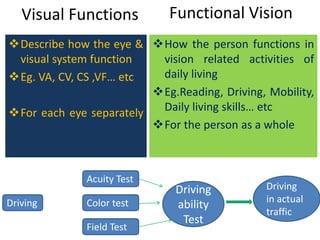
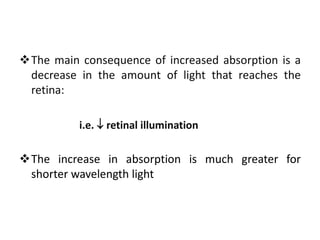
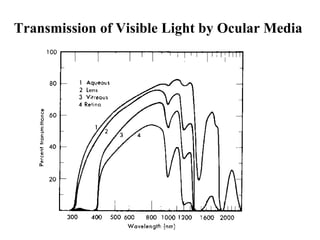
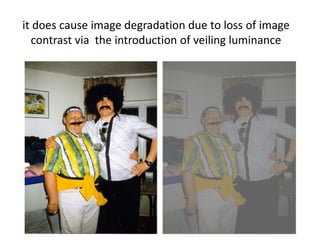
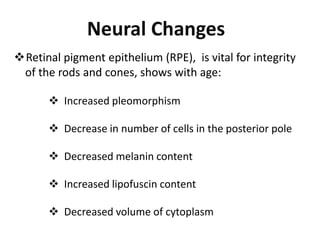
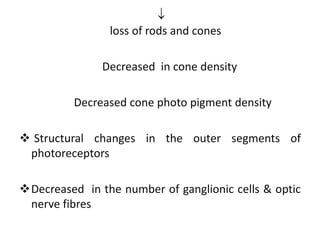
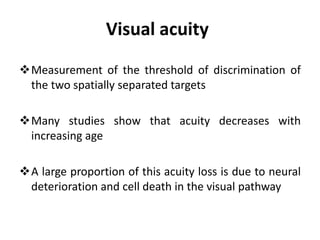
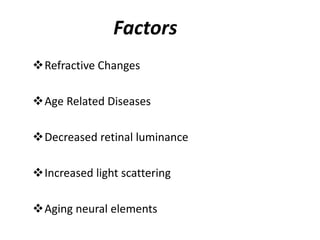
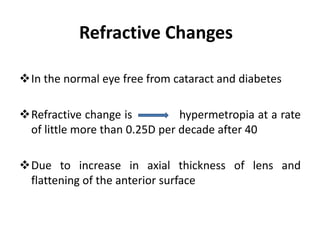
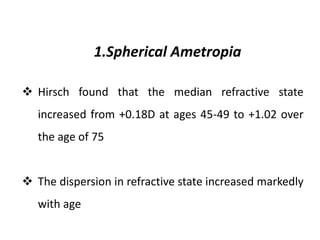
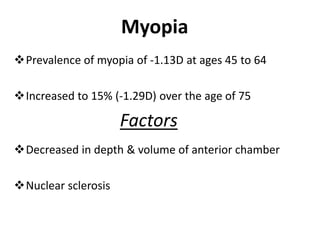
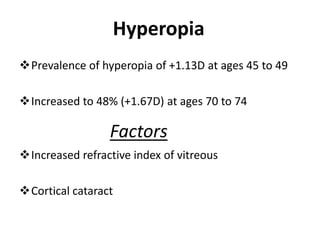
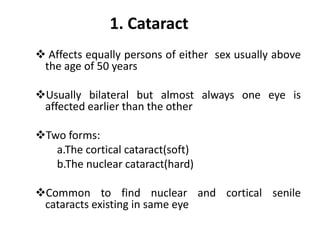
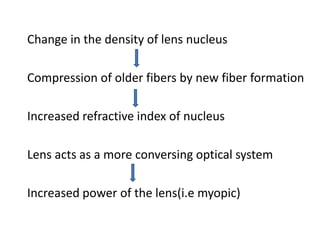
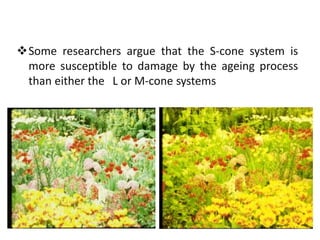
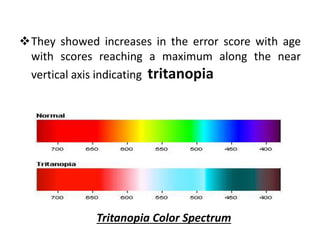
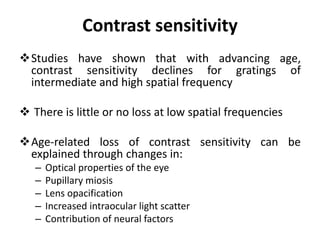
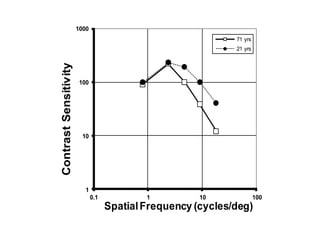
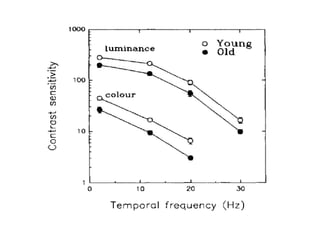
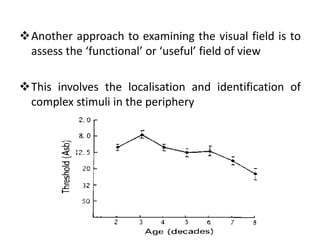
This document discusses how various visual functions change with age. It notes that as people age, their visual acuity, colour vision, contrast sensitivity, dark adaptation, visual fields and binocular vision typically deteriorate due to both optical and neural changes in the eye. Optical changes include increased light absorption and scattering by the lens, while neural changes involve loss of photoreceptors and ganglion cells. Common age-related eye diseases like cataracts, macular degeneration and diabetic retinopathy can also impair vision. The document outlines how each of these visual functions is specifically impacted by the aging process.