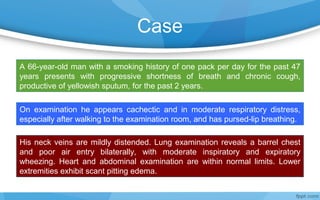
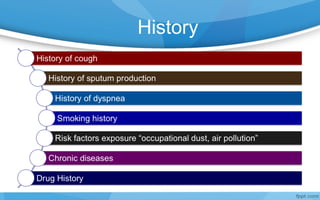
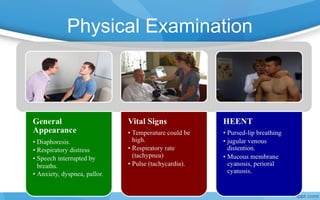
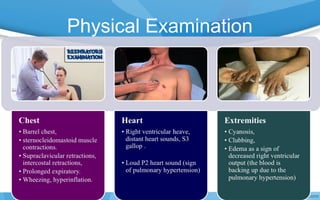
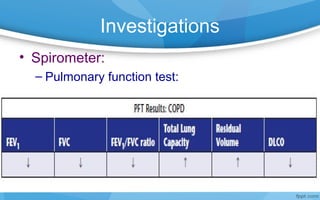
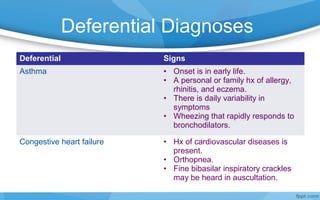
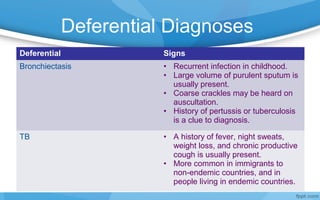
A 66-year-old man with a 47-year smoking history of one pack per day presents with progressive shortness of breath and chronic cough producing yellow sputum for two years. On examination, he has signs of respiratory distress, barrel chest, poor air entry, and wheezing. Spirometry shows airflow limitation consistent with COPD. Tobacco smoking is the main risk factor for COPD, causing inflammation, cilia dysfunction, and oxidative injury in the lungs. Differential diagnoses include asthma, congestive heart failure, bronchiectasis, and tuberculosis.