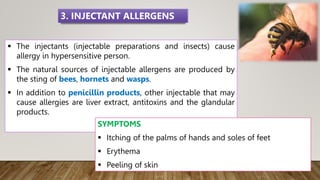
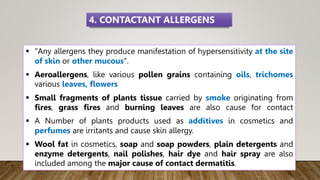
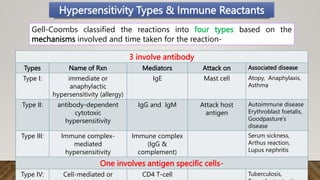
This document discusses different types of hypersensitivity reactions and allergies. It describes 4 types of hypersensitivity reactions:
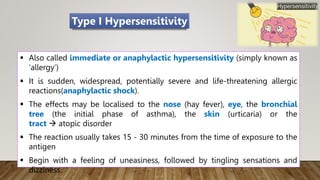
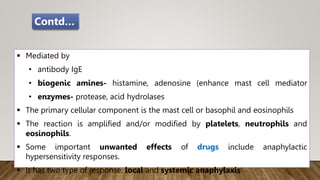
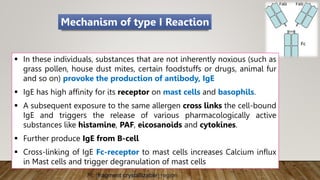
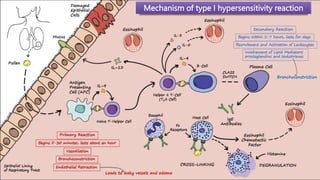
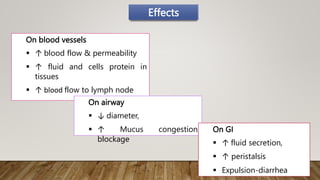
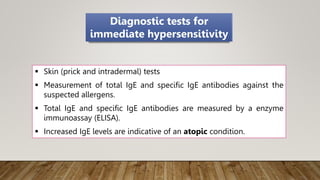
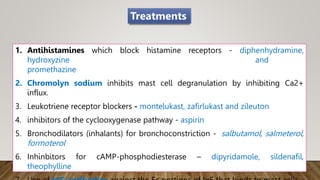
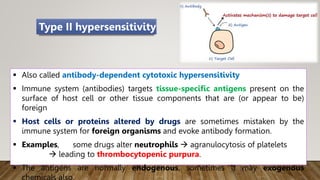
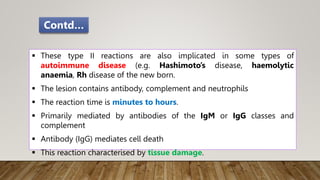
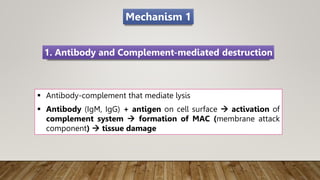
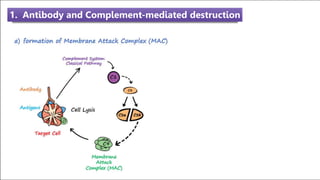
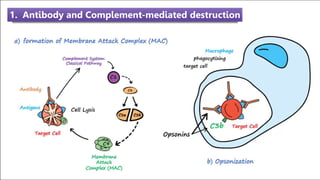
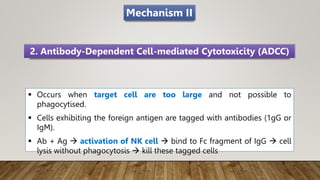
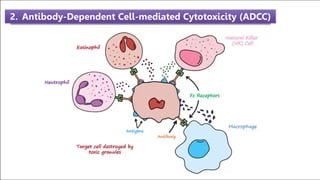
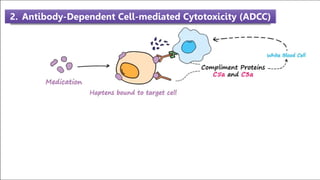
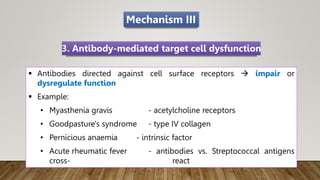
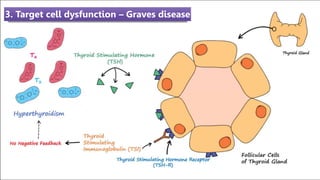
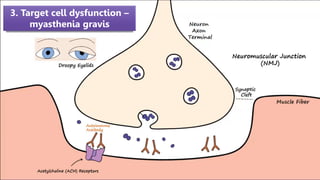
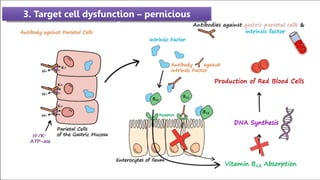
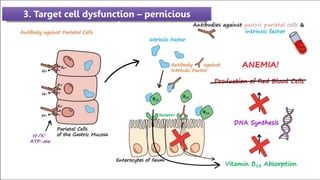
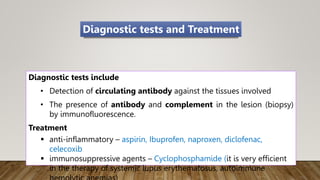
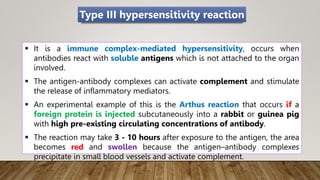
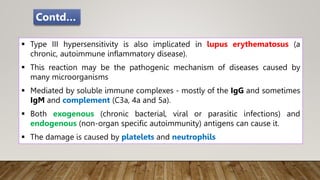
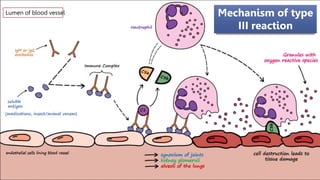
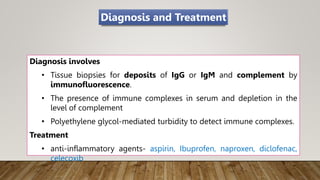
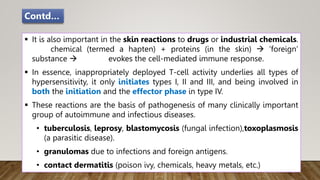
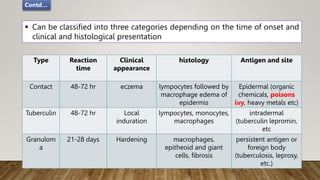
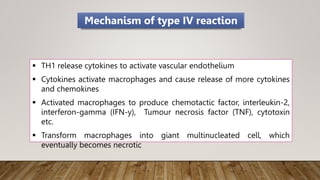
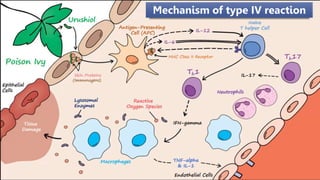
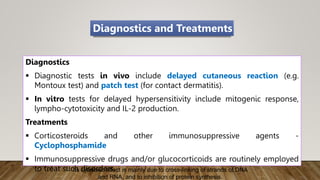
Type I is an immediate or anaphylactic reaction mediated by IgE antibodies and mast cells. Type II involves antibody-dependent cytotoxic reactions mediated by IgG and IgM antibodies. Type III reactions are immune complex-mediated responses. Type IV is a cell-mediated reaction involving T cells. The document provides details on the mechanisms, mediators, symptoms and treatments for each type of hypersensitivity reaction.