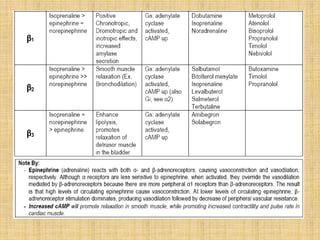
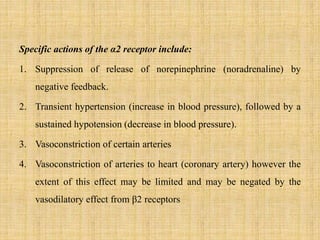
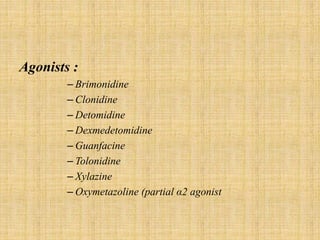
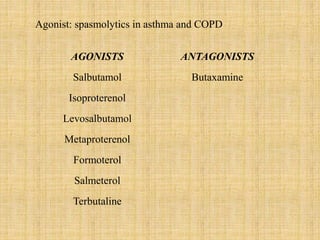
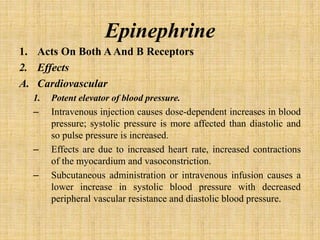
The adrenergic system involves proteins and drugs that interact with epinephrine and norepinephrine. Adrenergic receptors are membrane proteins targeted by these hormones, while transporters carry norepinephrine across cell membranes. Agonists produce similar effects and antagonists block effects.
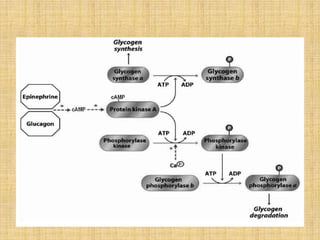
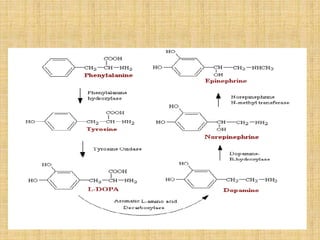
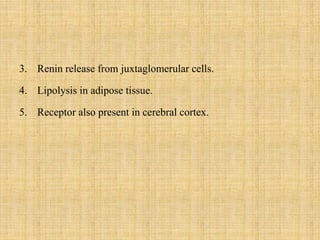
Epinephrine and norepinephrine act as hormones and neurotransmitters, regulating processes like smooth muscle contraction and increased blood pressure/glucose levels. Norepinephrine is synthesized in nerve cells and stored in vesicles for release. It initiates the fight-or-flight response through alpha and beta receptors in various tissues.