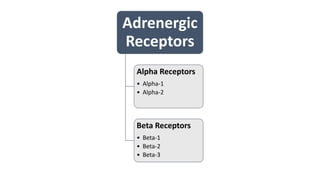
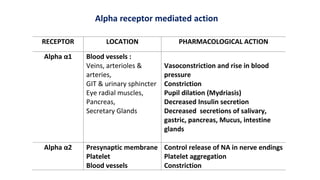
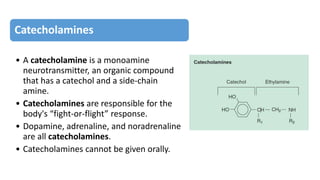
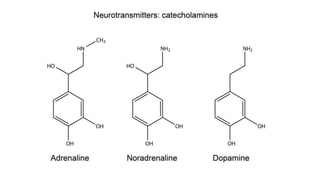
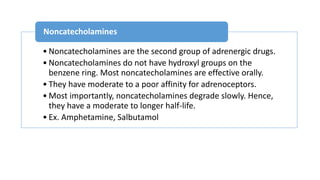
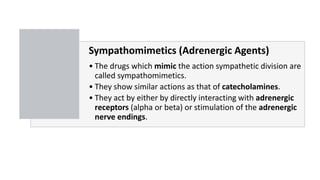
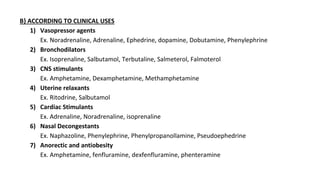
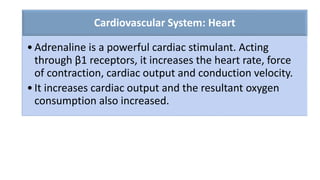
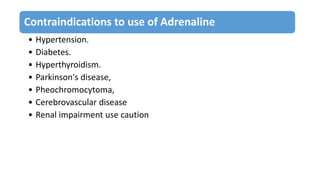
The document provides a detailed overview of the sympathetic nervous system and sympathomimetics, emphasizing its role in the 'fight or flight' response, neurotransmission mechanics, and the pharmacological actions of associated drugs. It categorizes sympathomimetic drugs by their mechanism of action and clinical applications, such as vasopressors and bronchodilators. Additionally, the document discusses catecholamines, their effects on various systems, and potential adverse effects, underscoring the importance of proper usage and contraindications.