1) The document discusses the lymphatic and immune systems, including lymphoid organs, lymphocytes, antigen presentation, and the major histocompatibility complex.
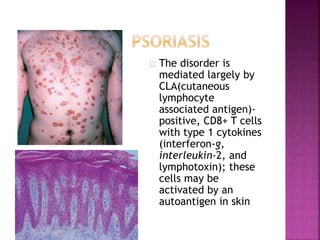
2) It describes T lymphocyte development and function, including the roles of CD4+ and CD8+ T cells.
3) The roles of B lymphocytes and antibody production are summarized.