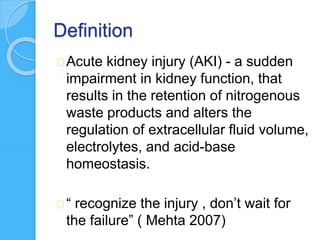
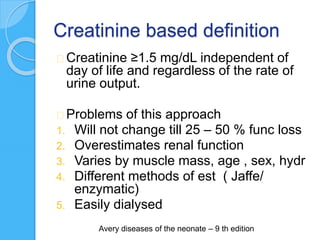
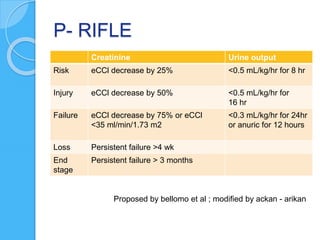
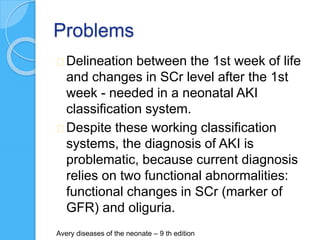
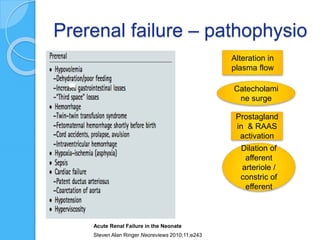
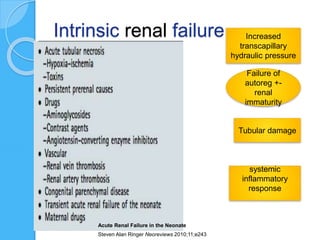
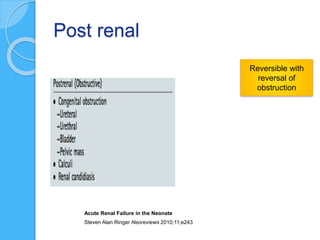
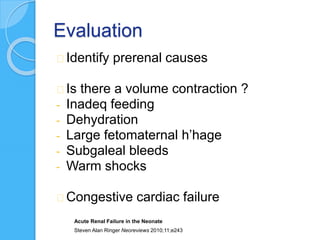
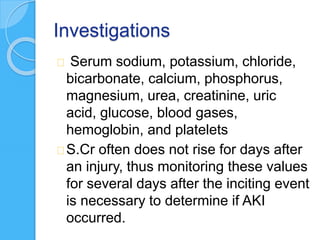
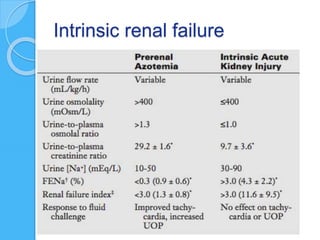
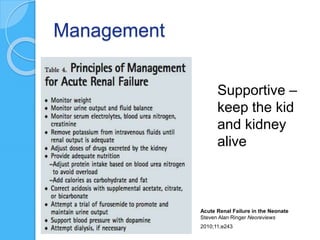
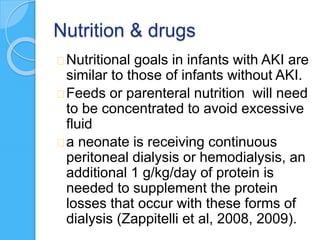
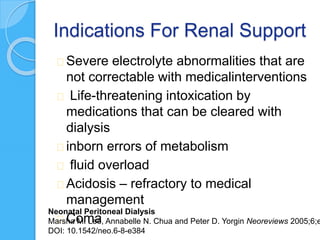
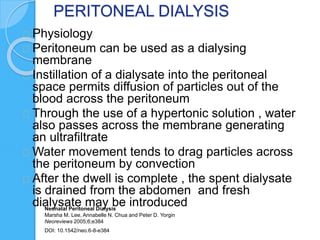
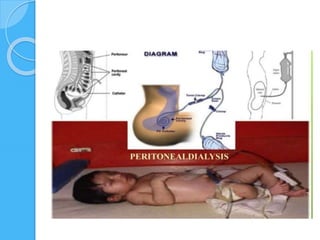
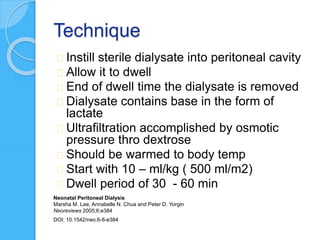
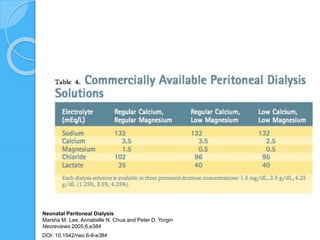
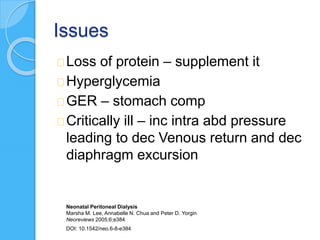
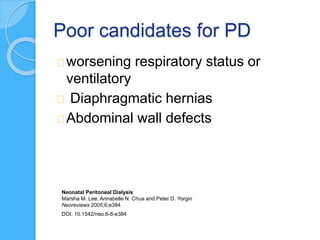
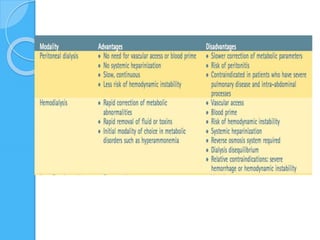
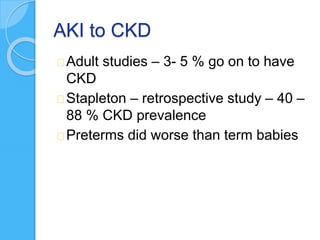
AKI in neonates can be caused by prerenal, intrinsic renal, or postrenal factors. It is defined and classified using creatinine and urine output criteria. Management involves identifying and treating the underlying cause, maintaining fluid/electrolyte balance, and considering renal replacement therapy for refractory cases. Peritoneal dialysis is often preferred for neonates as it is gentler than hemodialysis and can provide both fluid removal and metabolic control. However, peritoneal dialysis also carries risks of peritonitis, mechanical issues, and complications in critically ill infants.