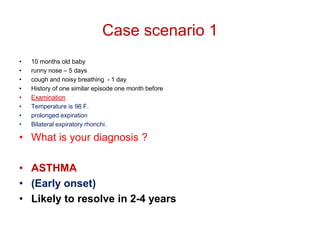
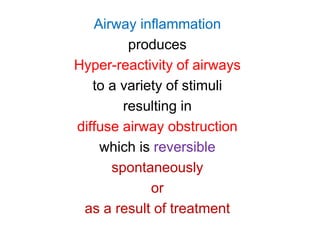
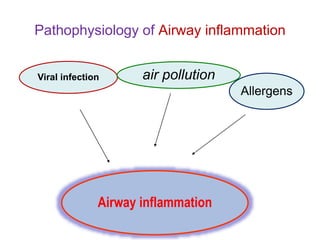
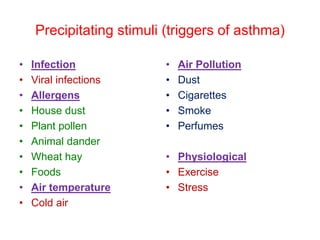
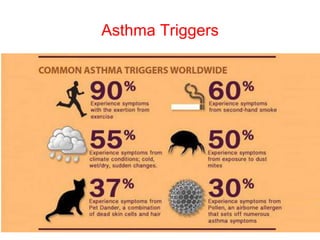
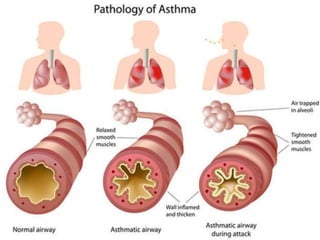
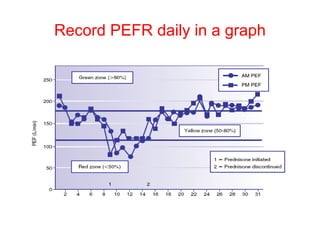
This document discusses childhood asthma, including its classification, epidemiology, etiology, pathogenesis, clinical features, complications, management, prognosis, and prevention. It provides case scenarios to demonstrate the diagnosis of asthma in children. Key points include that asthma is a chronic inflammatory condition of the airways causing episodic obstruction, it has a prevalence of 20% in Pakistani children, and is diagnosed based on a history of recurrent or intermittent respiratory symptoms and signs of bronchial obstruction on examination. Asthma is managed by avoiding triggers, using quick-relief and preventive medications, and treating exacerbations.