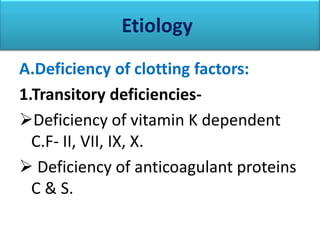
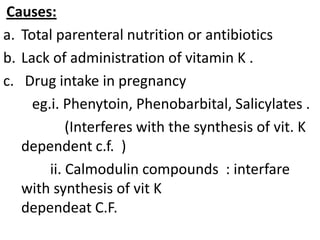
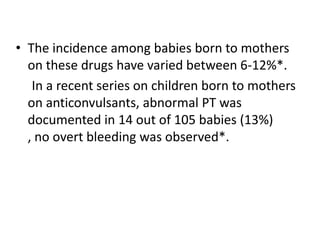
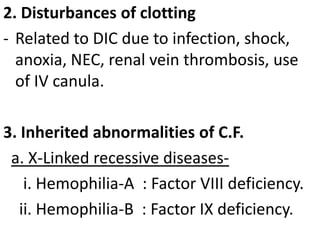
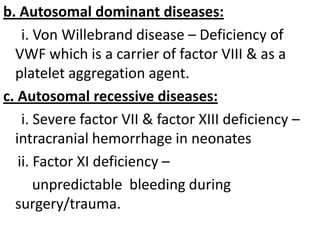
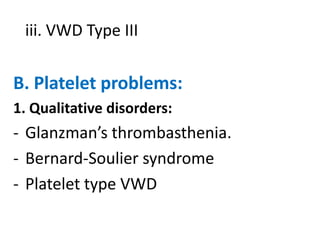
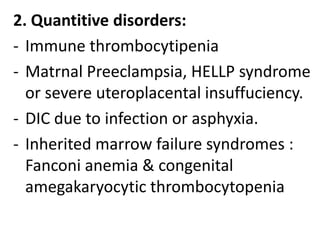
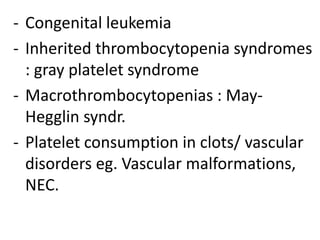
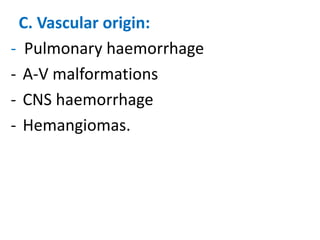
1) A bleeding neonate can have deficiencies in clotting factors or platelets due to various causes such as lack of vitamin K, maternal medication exposure, or inherited conditions.
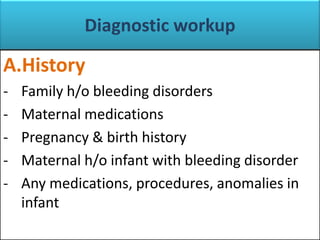
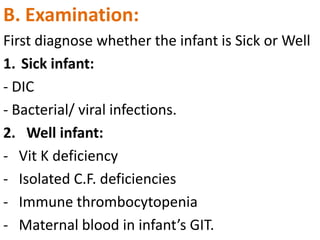
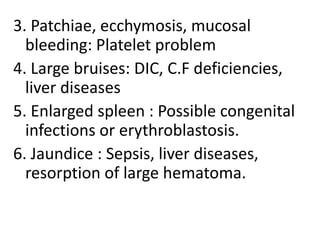
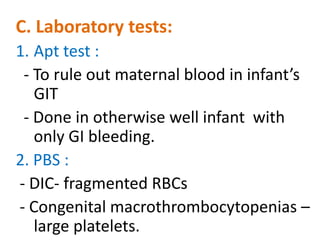
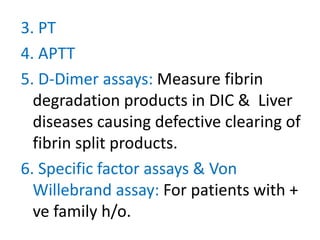
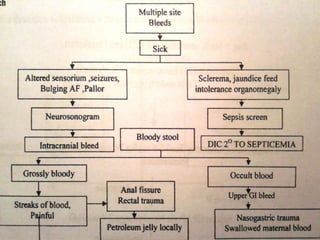
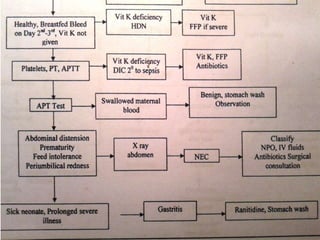
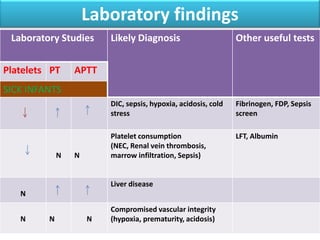
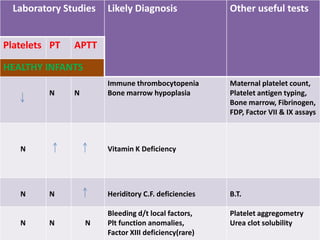
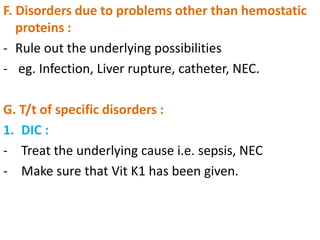
2) Evaluation involves examining the infant's history and health status to determine if signs point to a systemic problem or isolated clotting issue, and performing lab tests like PT, PTT, and factor assays.
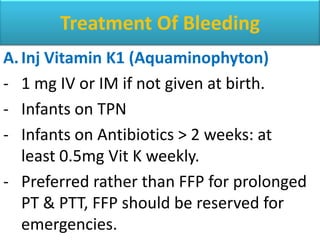
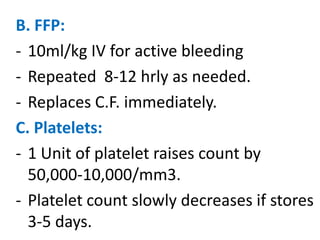
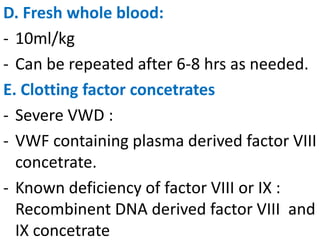
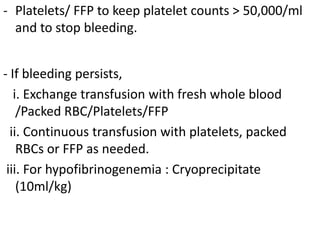
3) Treatment depends on the underlying etiology but may include vitamin K, fresh frozen plasma, platelets, or specific clotting factor concentrates. Ongoing care and monitoring is important for managing inherited bleeding disorders or diseases.