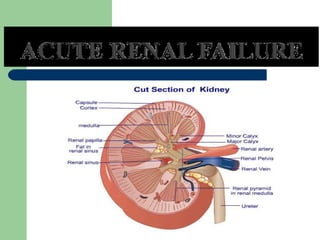
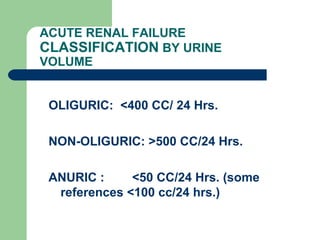
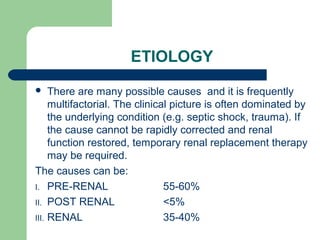
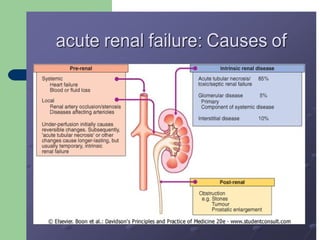
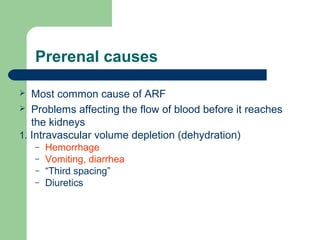
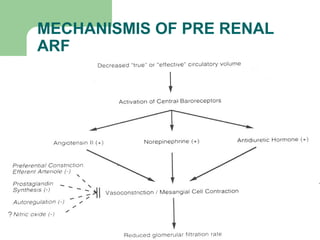
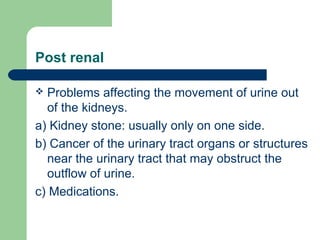
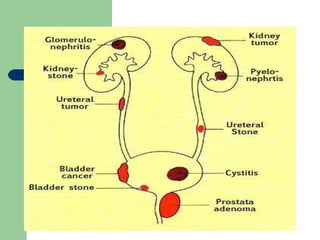
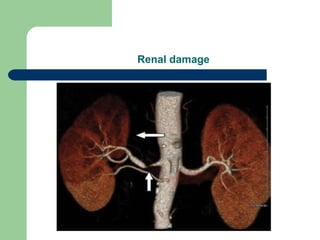
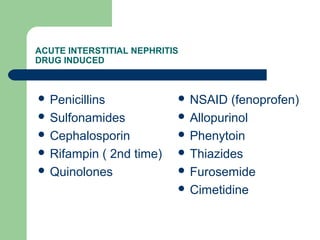
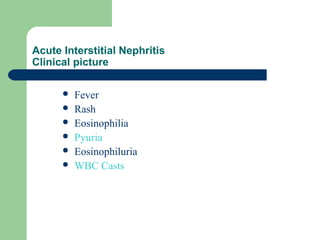
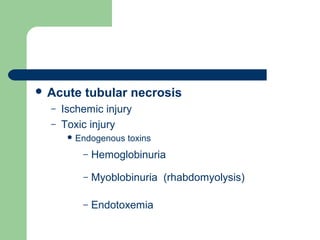
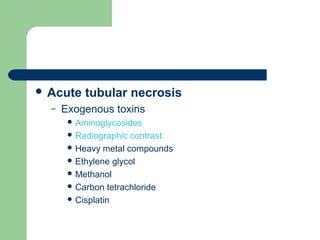
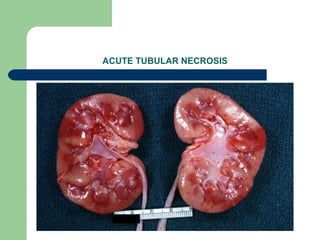
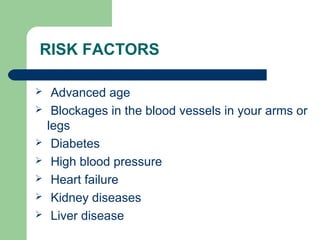
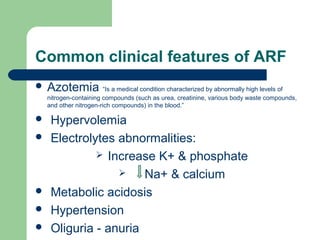
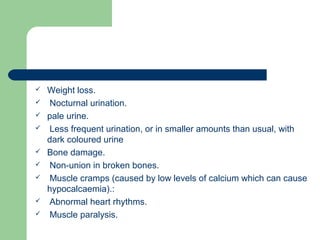
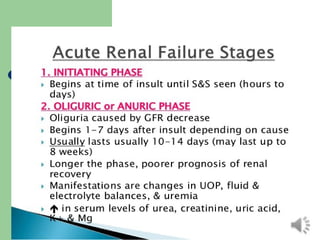
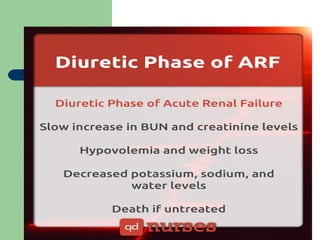
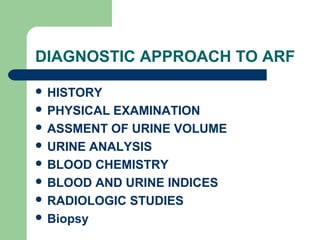
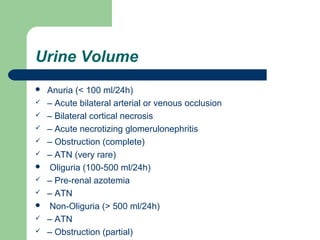
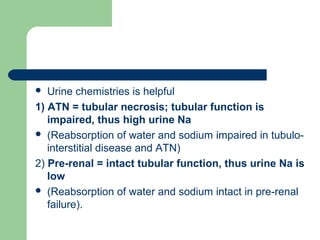
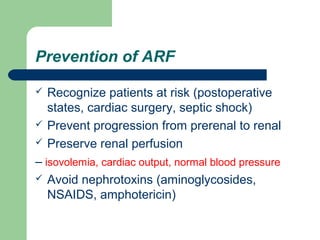
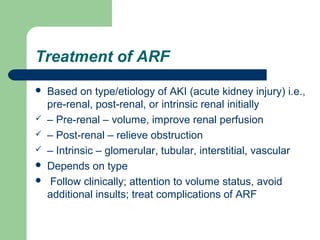
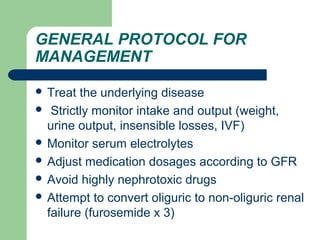
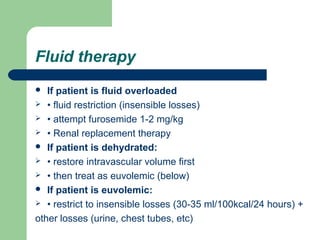
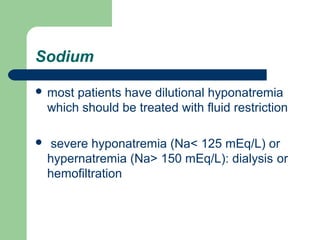
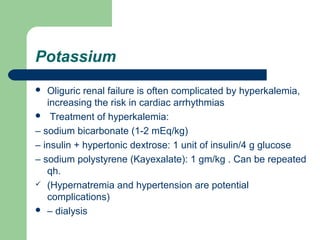
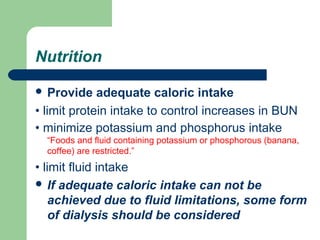
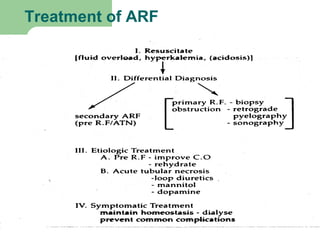
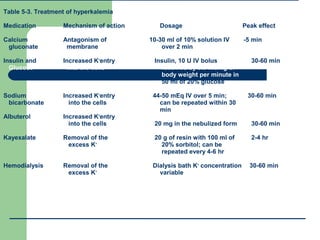
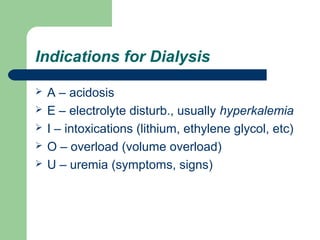
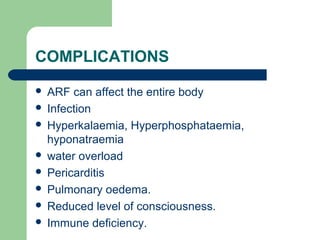
The document discusses acute renal failure (ARF), defining it as a sudden reduction in kidney function that results in waste accumulating in the blood. It classifies ARF by urine volume and lists the main causes as pre-renal, post-renal, and renal. Pre-renal causes include volume depletion and problems with blood flow. Post-renal causes involve urine outflow issues. Renal causes include tubular necrosis, interstitial nephritis, and glomerular disease. The document provides details on evaluating and managing ARF, including through fluid management, treating electrolyte abnormalities, and considering renal replacement therapy.



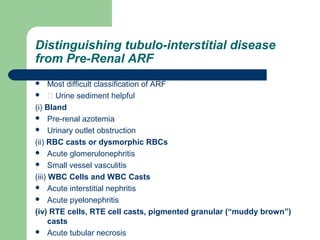
![ARF -- Summary
Dx AKI by falling GFR [rising BUN and
creatinine]
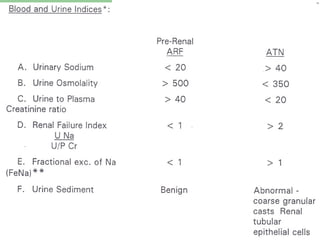
Classify into pre-renal, renal, or postrenal by
history, PE, BUN:creat ratio, urine analysis
Sometimes also need urine chemistries [urine
Na, FxExNa and/or FxExurea] to distinguish
pre-renal from ATN.](https://image.slidesharecdn.com/arfbyabdinur-180218153106/85/Acute-Renal-failure-57-320.jpg)
![ARF – Summary (cont…)
Sometimes need renal ultrasound to verify
obstruction [post-renal ARF]
Rarely need other studies, esp to dx type of
intrinsic ARF [e.g., kidney biopsy: GN vs
interstitial nephritis vs ATN].](https://image.slidesharecdn.com/arfbyabdinur-180218153106/85/Acute-Renal-failure-58-320.jpg)