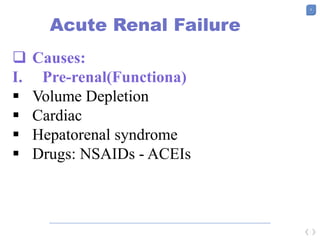
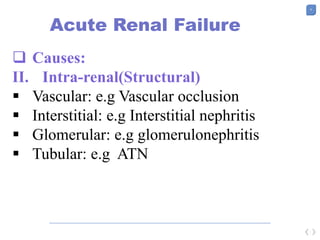
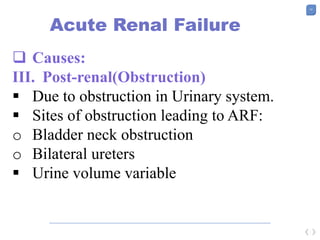
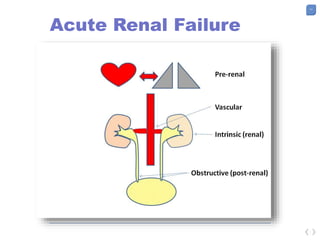
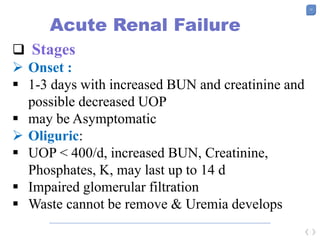
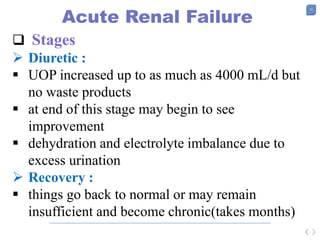
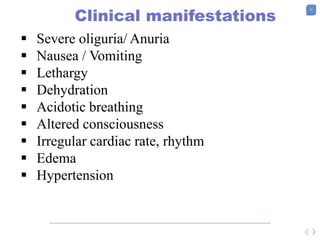
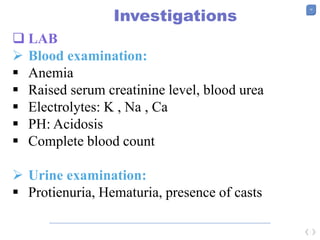
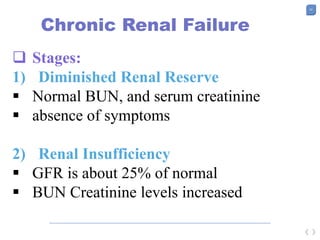
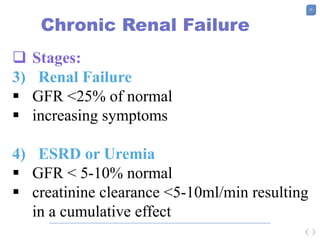
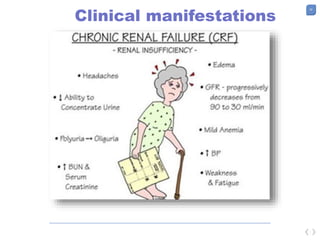
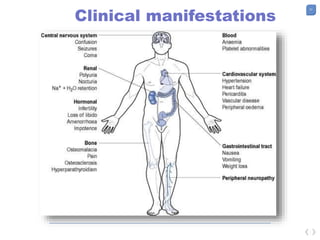
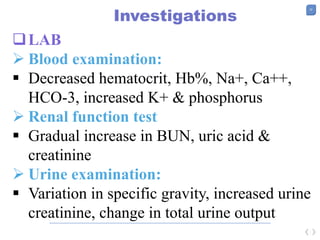
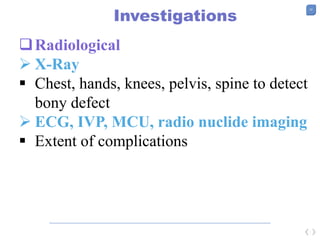
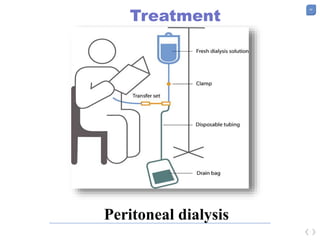
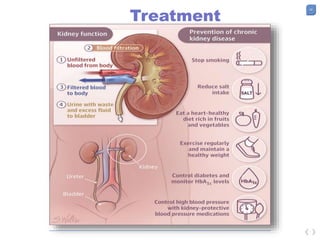
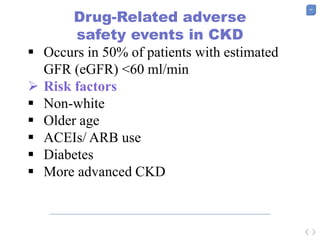
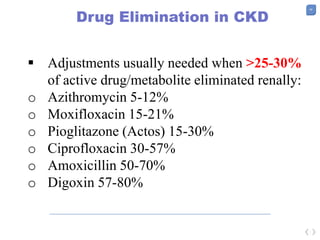
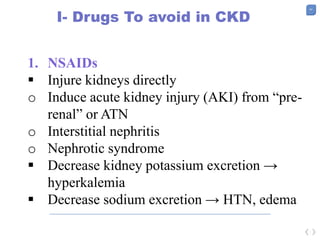
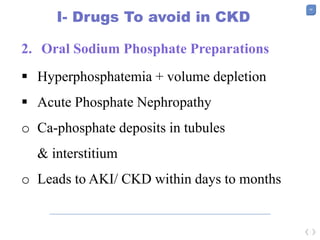
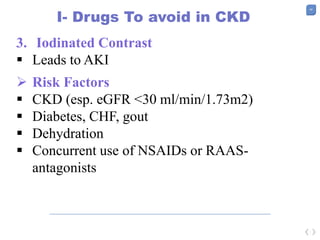
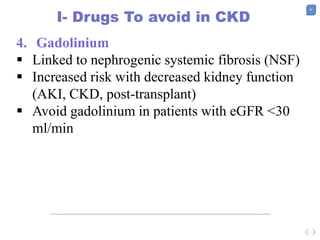
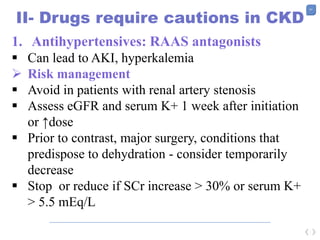
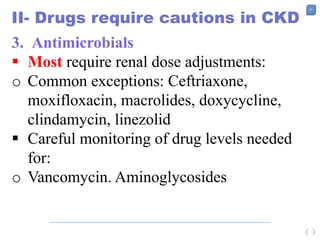
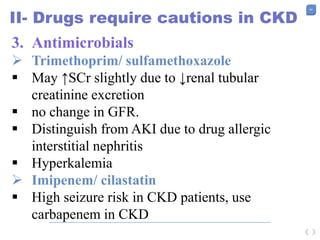
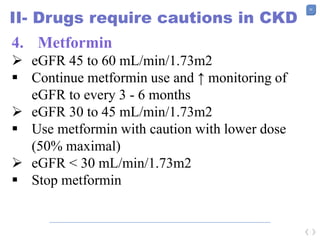
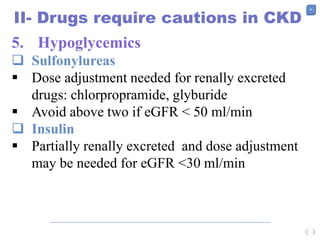
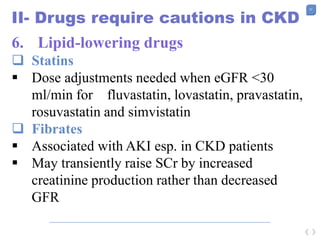
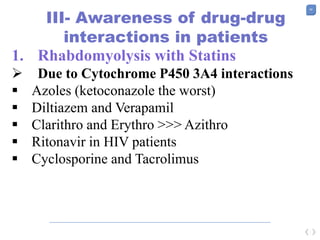
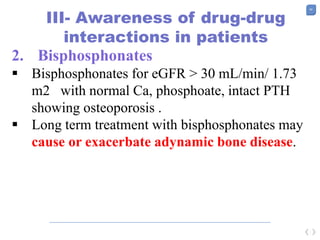
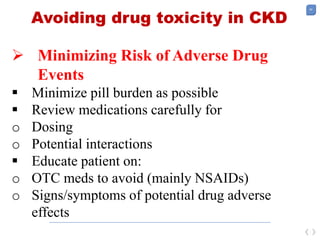
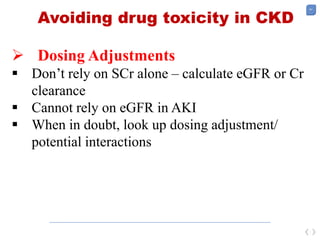
The document discusses the management of renal failure, detailing acute and chronic renal failure, their causes, clinical manifestations, and treatment options. Acute renal failure is characterized by rapid kidney function loss, while chronic renal failure involves irreversible nephron destruction. The document also highlights drug safety in chronic kidney disease, emphasizing necessary adjustments and drugs to avoid due to their risk of toxicity.