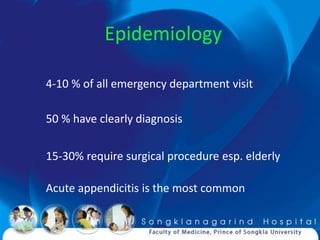
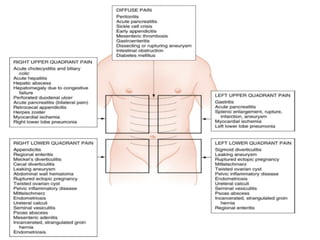
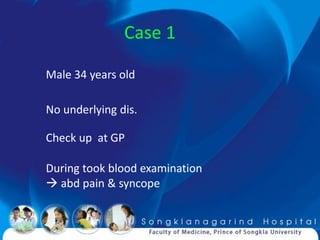
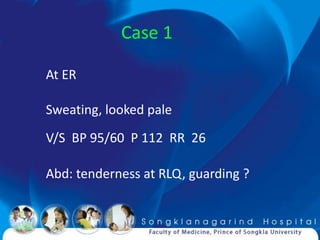
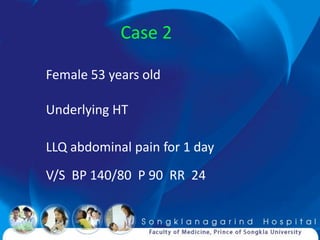
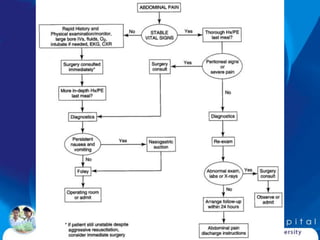
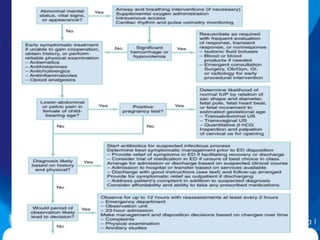
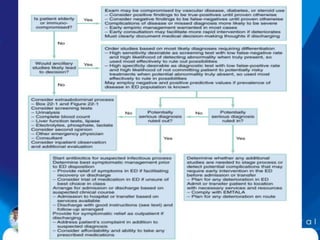
1) Acute abdomen is a common presentation accounting for 4-10% of emergency department visits. 50% have a clear diagnosis while 15-30% require surgical procedures, especially in the elderly.
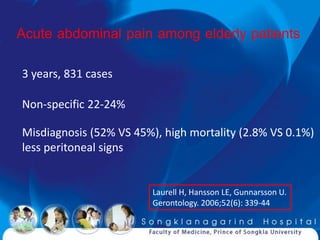
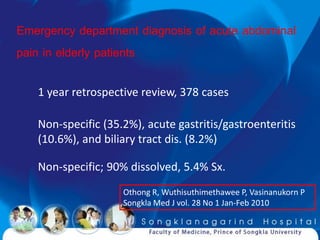
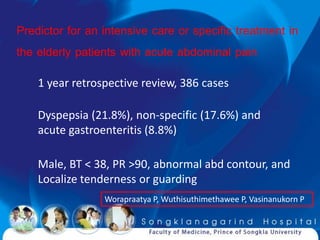
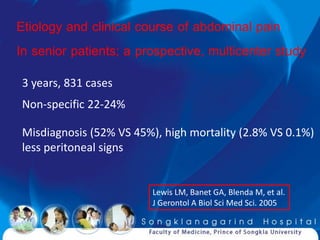
2) Unique presentations can occur in pediatric and elderly patients, with the elderly having higher rates of misdiagnosis and mortality due to less prominent physical exam findings.
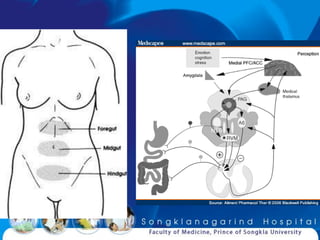
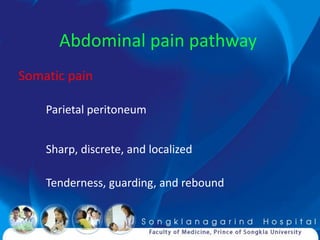
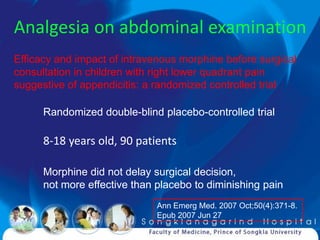
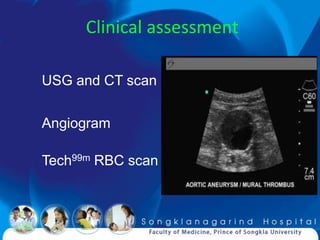
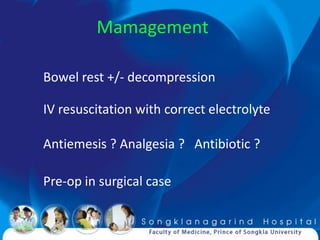
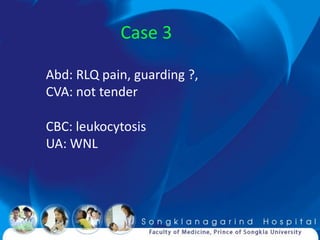
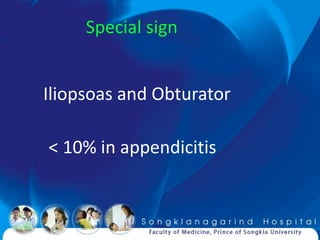
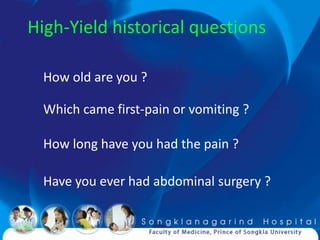
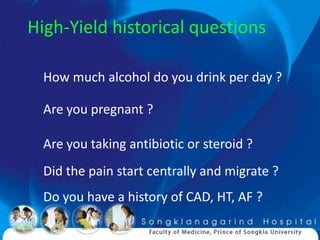
3) A thorough history and physical exam remain important for assessing abdominal pain, though imaging studies can help when the diagnosis is unclear. Close observation is often needed to determine if the condition is surgical or non-surgical.