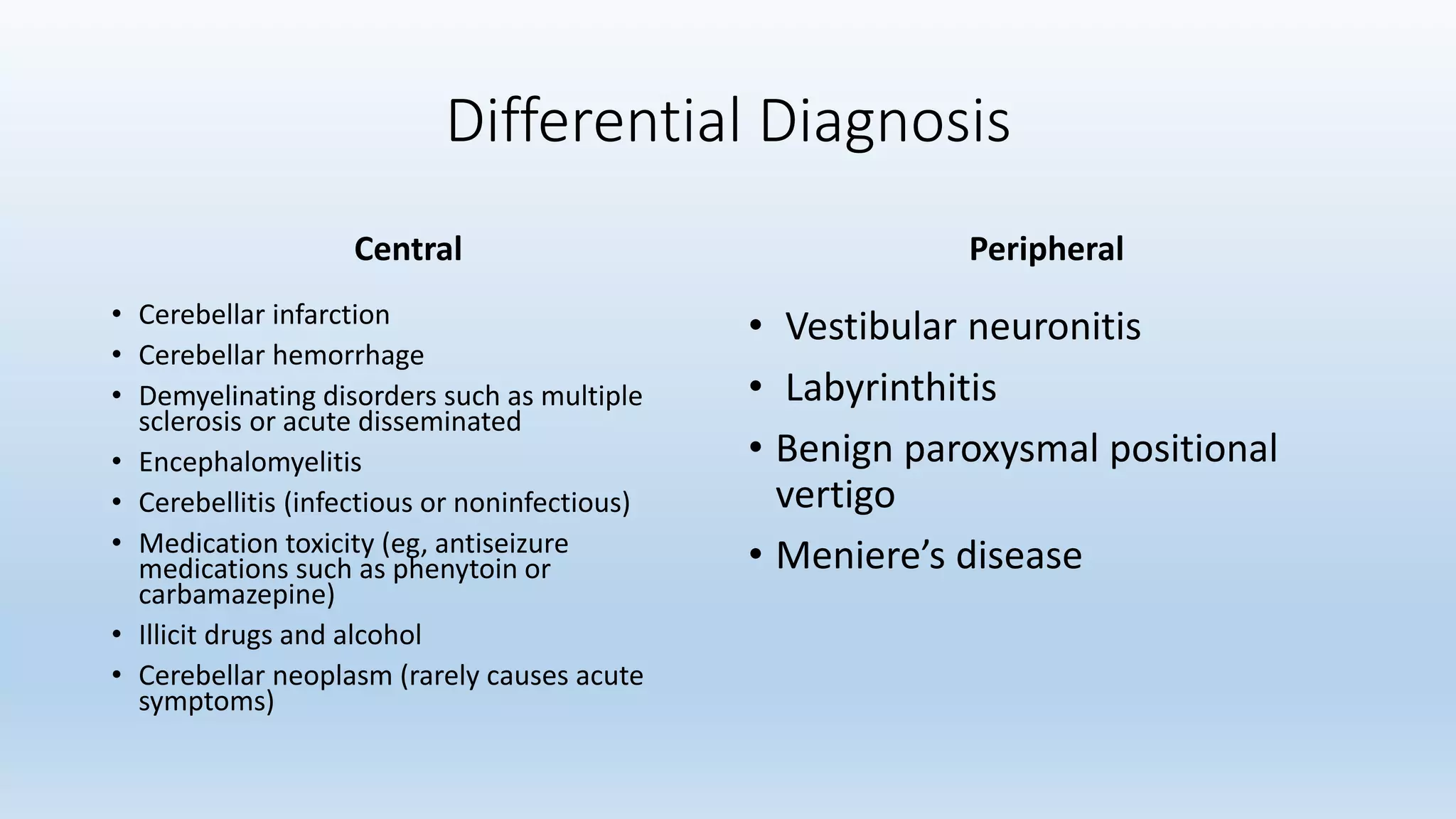
Cerebellar infarction is a rare type of stroke accounting for 2-3% of cases. It can cause serious complications due to the cerebellum's location. Symptoms include nausea, vomiting, dizziness and headache. Common causes are cardiac embolism, atherosclerosis and arterial dissection. Complications include swelling, mass effect and brainstem compression. Patients require close monitoring and may need decompressive surgery. With proper management, prognosis can be good in the absence of additional brainstem injury.