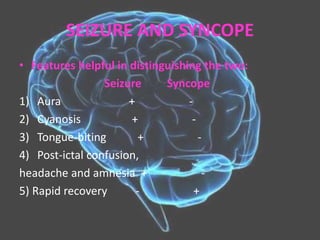
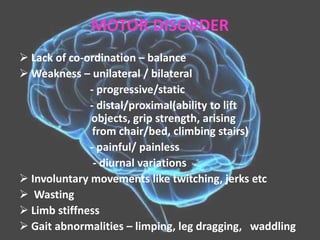
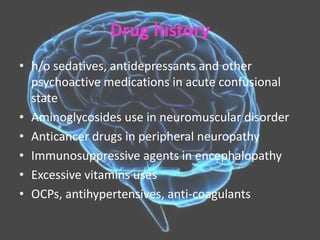
The document provides guidance on neurological history taking. It outlines the necessary prerequisites, proforma, goals, and descriptions for evaluating common neurological presentations such as headache, visual disturbances, loss of consciousness, seizures, speech and motor disorders, sensory changes, and alterations in mental state. Key areas of history include onset, duration, frequency and characteristics of symptoms, as well as family, personal, medical and medication histories. A thorough neurological examination aims to localize lesions in the nervous system and determine the nature of any pathology.