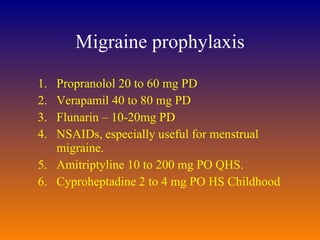
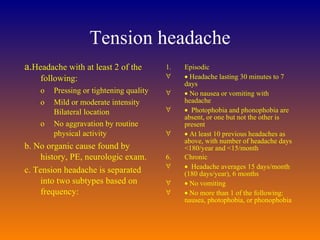
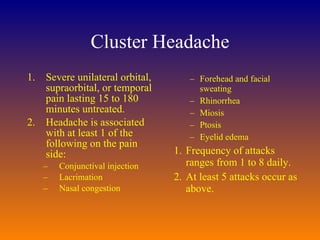
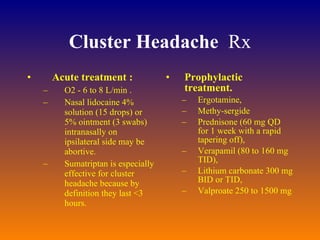
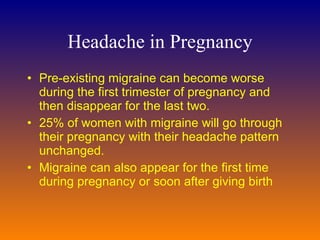
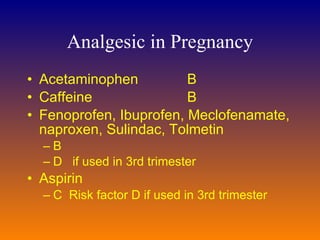
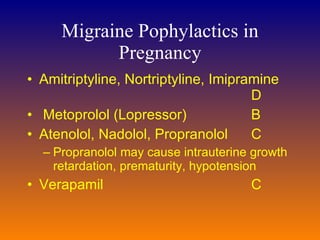
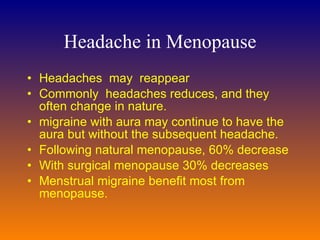
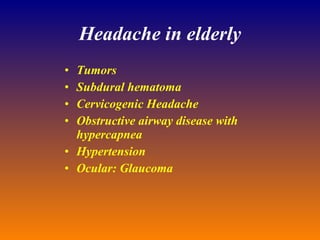
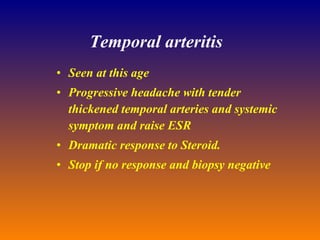
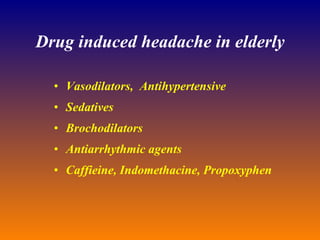
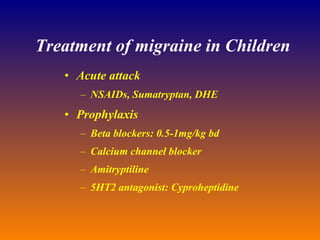
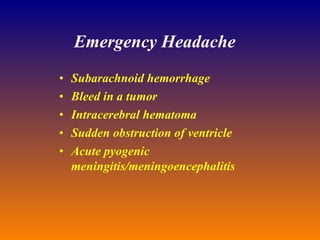
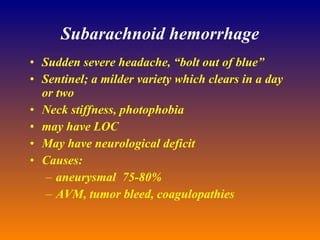
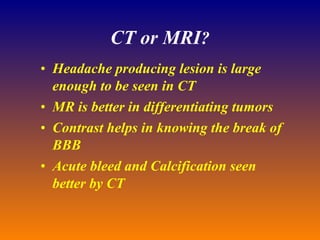
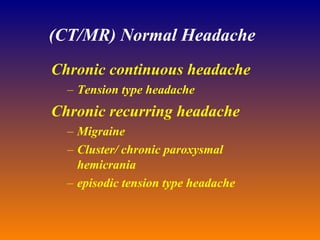
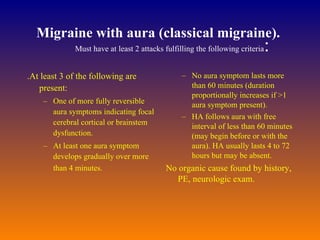
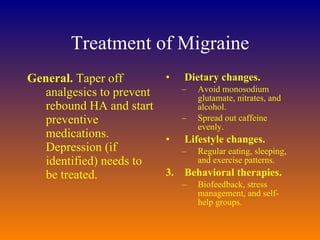
This document provides an overview of headache management in family practice. It discusses evaluating and treating common headache types like migraine, tension headache, and cluster headache. It covers diagnostic testing, acute and preventive treatment options, and considerations for headache in special populations like pregnancy, menopause, and the elderly.



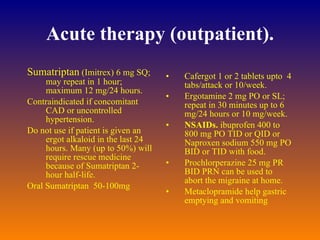
![Acute therapy - Migraine Prochlorperazine 10 mg IV. Metoclopramide 5 to 10 mg IV Q8h. Often given with dihydroergotamine (DHE) to prevent DHE-induced nausea. May be combined orally with ASA. NSAIDs (ketorolac [Toradol] 60 mg IM, Dihydroergotamine (DHE) 0.75 mg IV Meperidine 50 to 100 mg IM Q3h PRN. Dexamethasone 4 mg IM or a short course of prednisone (40 to 60 mg PO QD), combined with analgesics above, if migraine continues >24 hours. Sumatriptan (Imitrex); see above for dose. Oral sumatriptan also available but less effective.](https://image.slidesharecdn.com/headachemanagement11thfeb2001-100618010919-phpapp01/85/Headache-management-21-320.jpg)