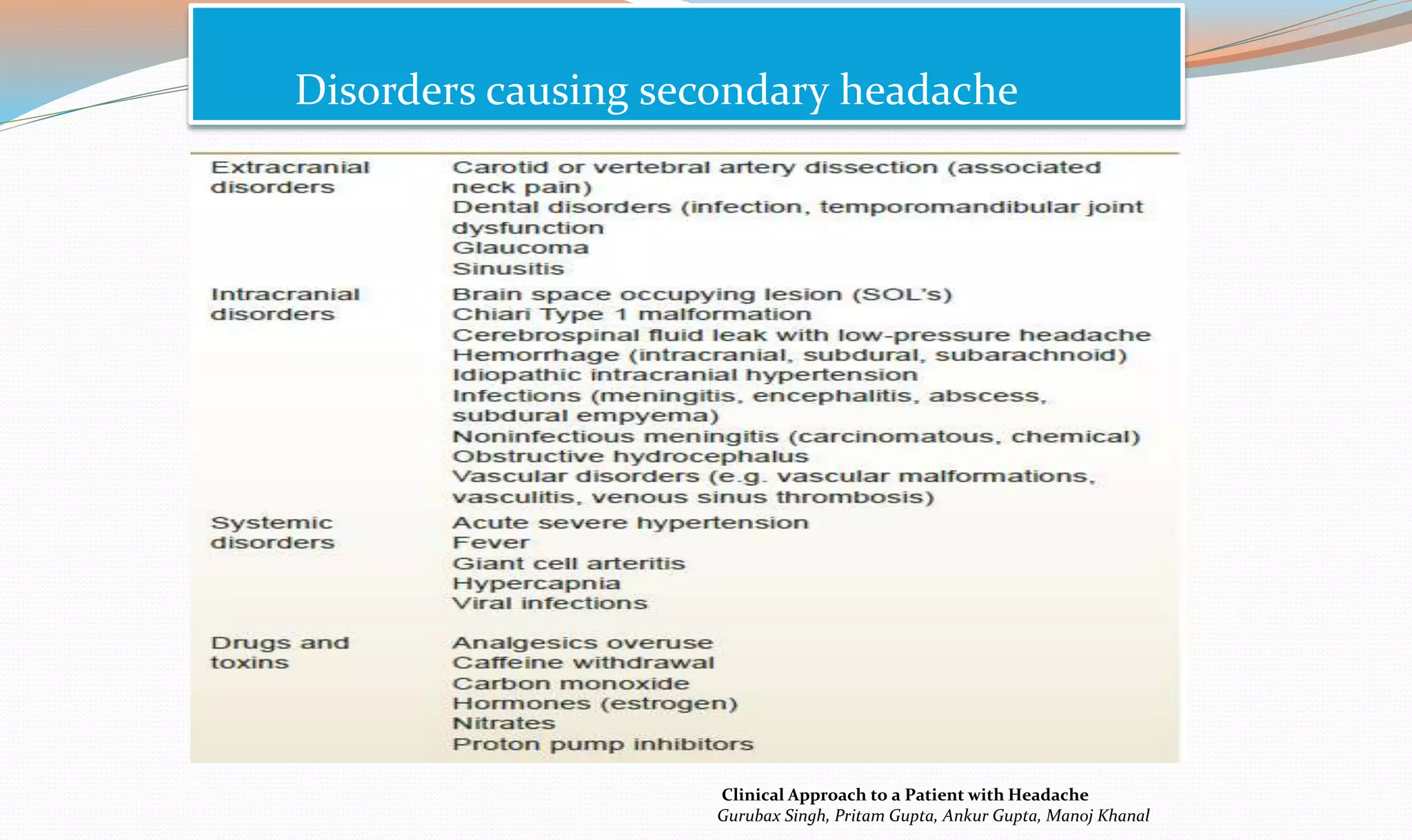
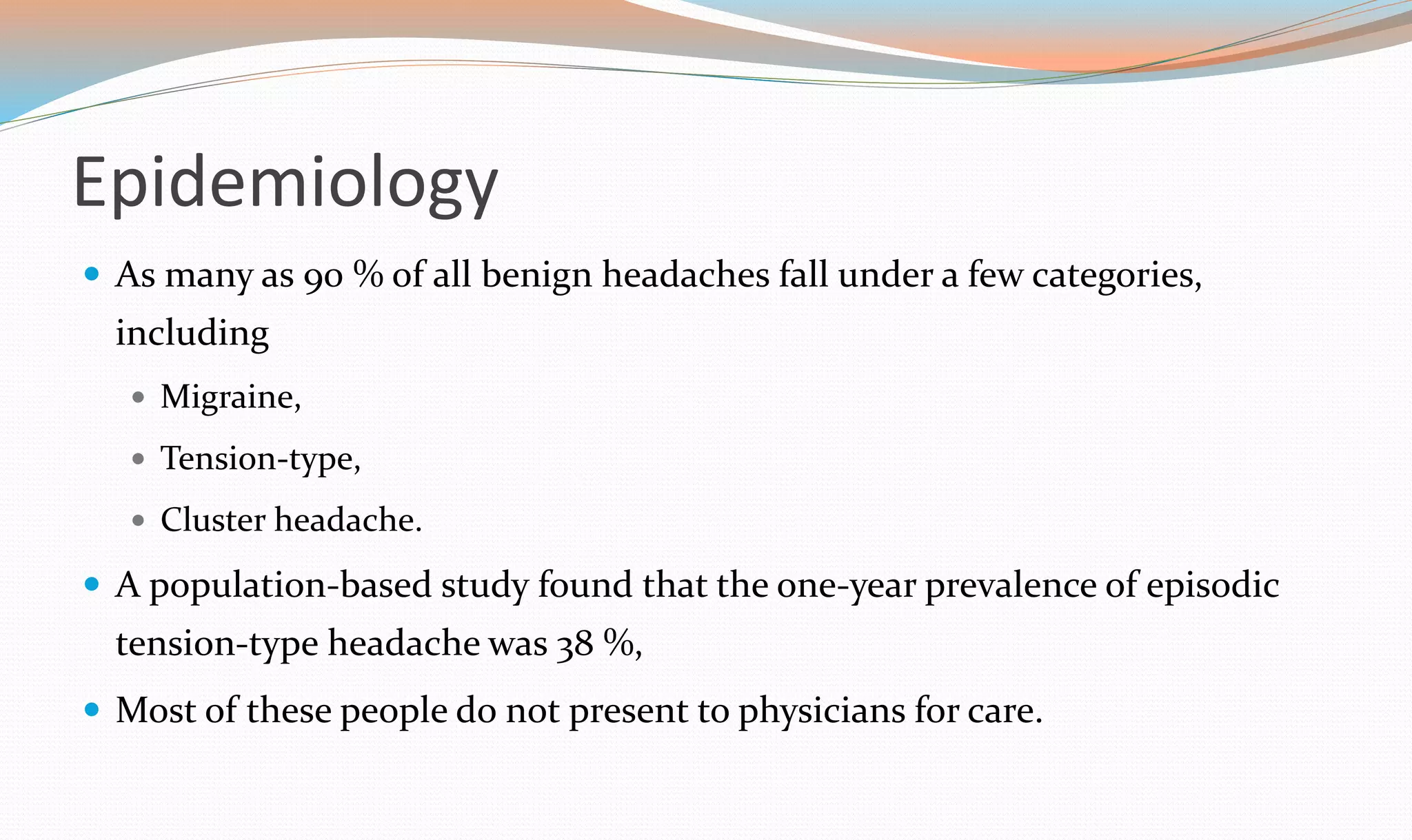
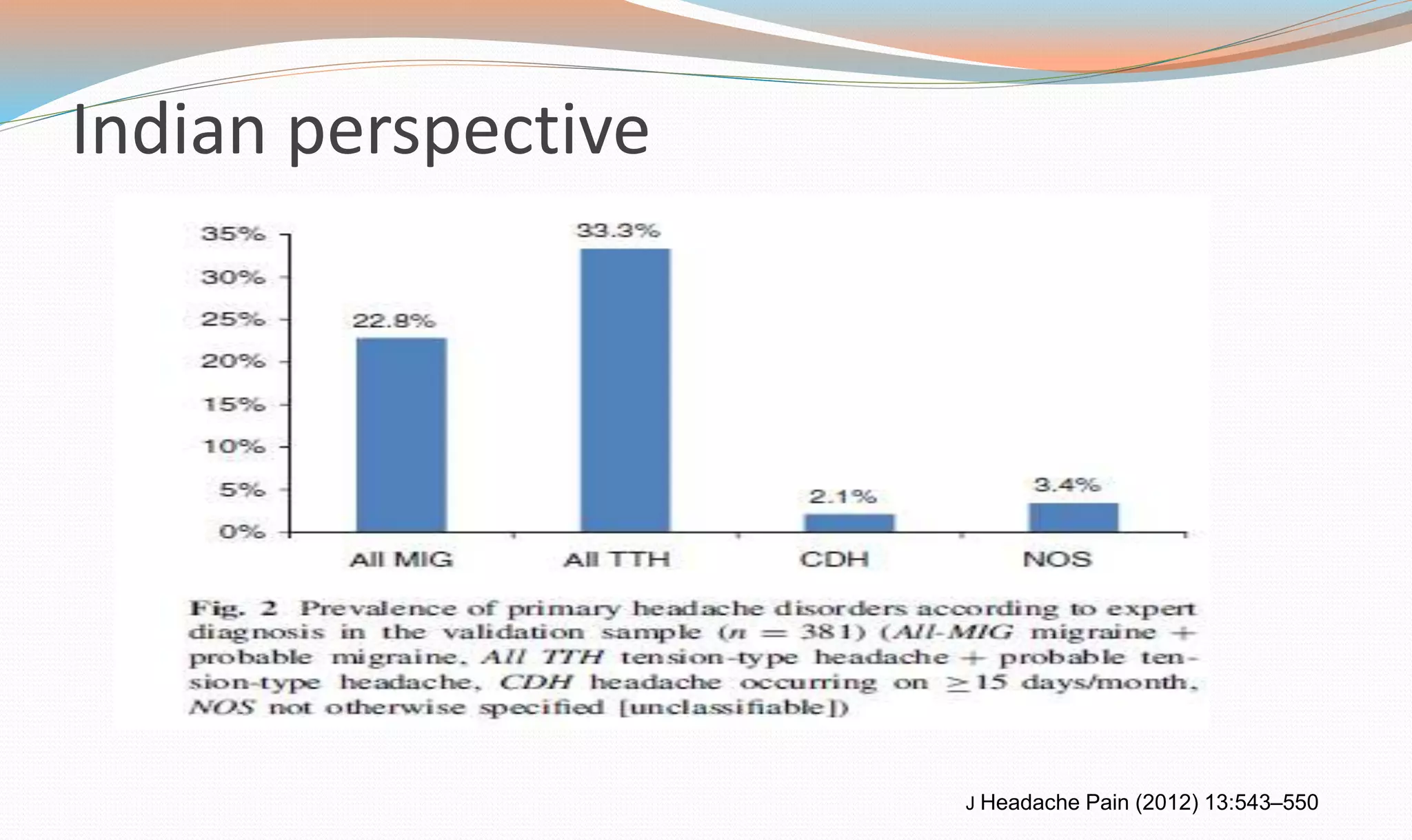
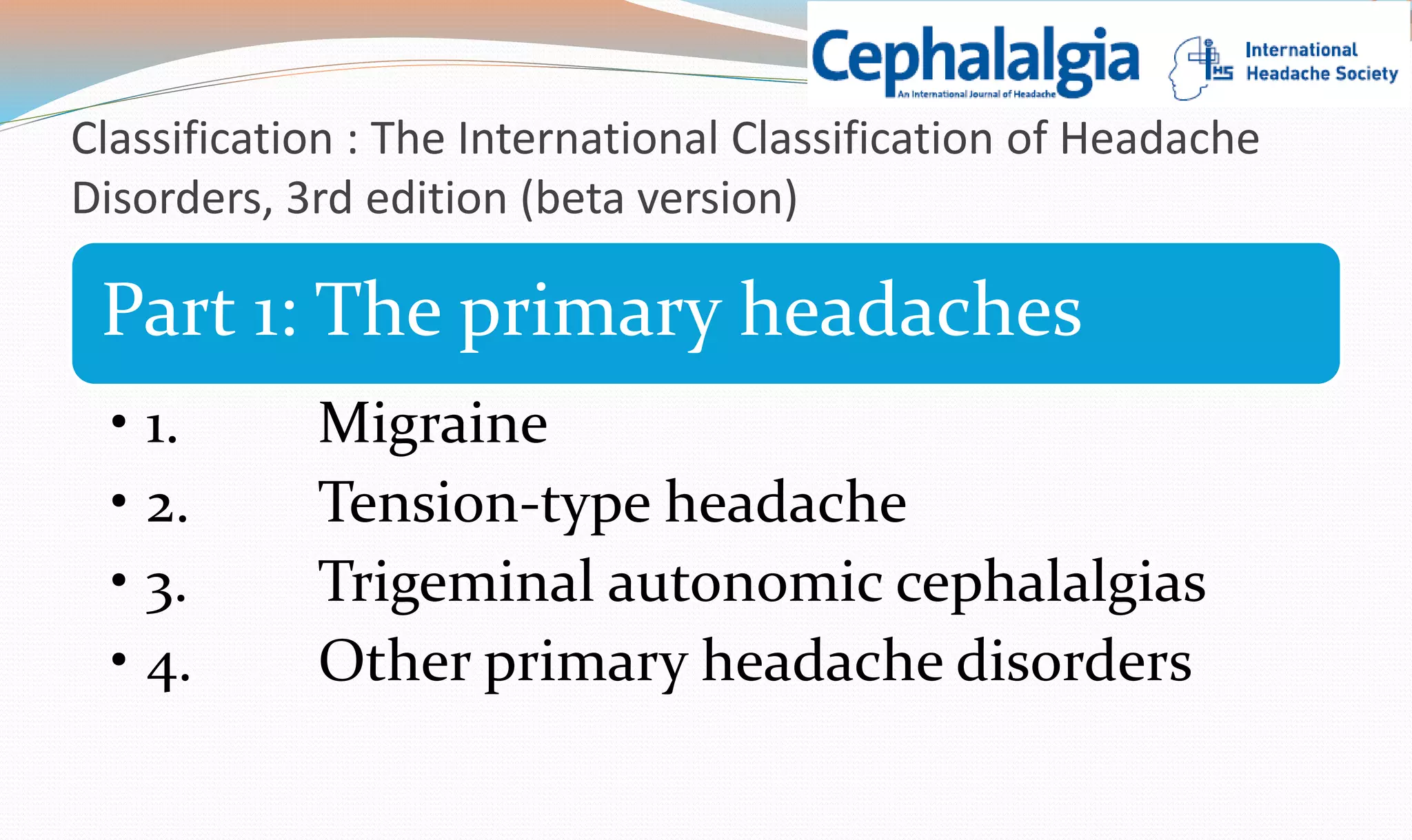
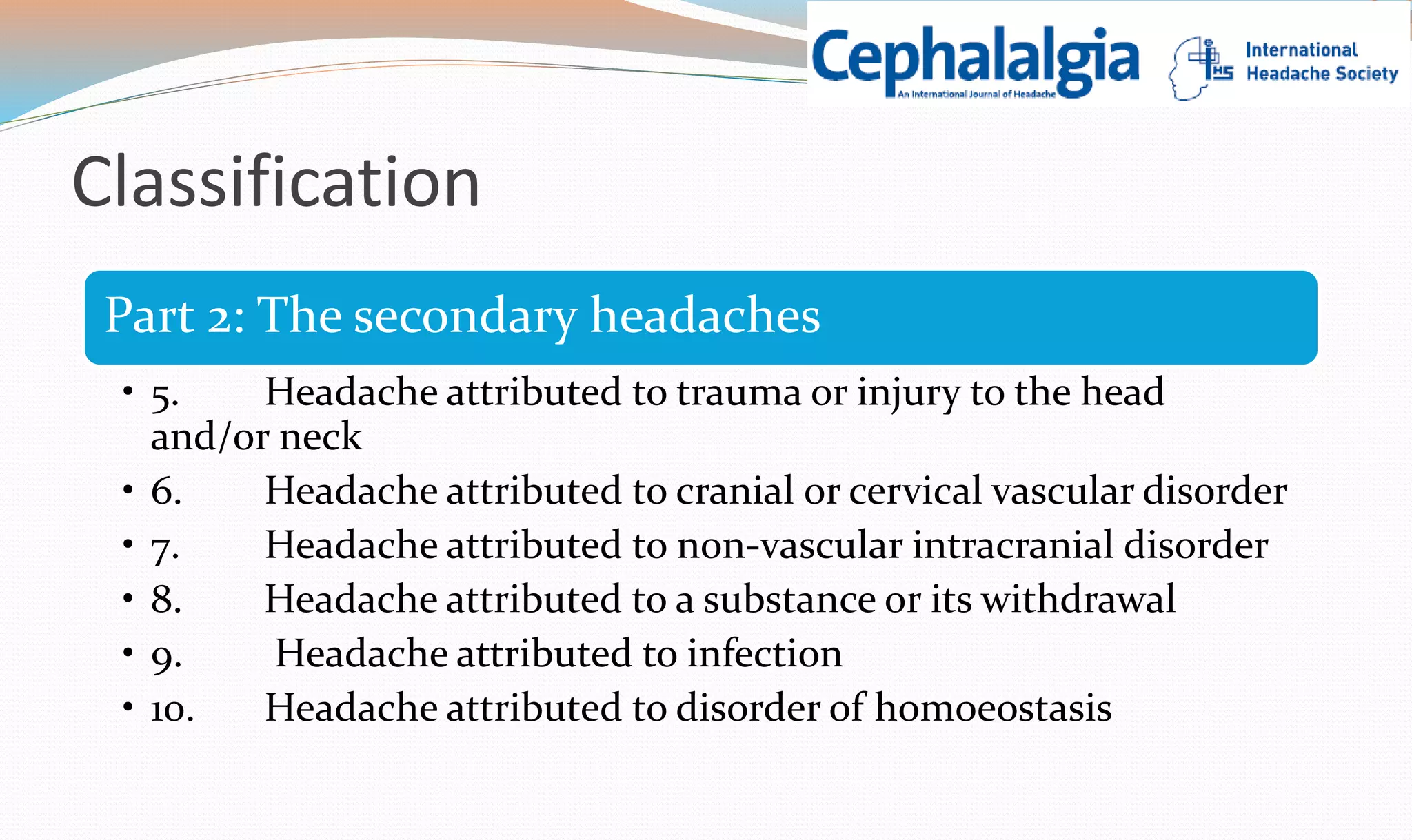
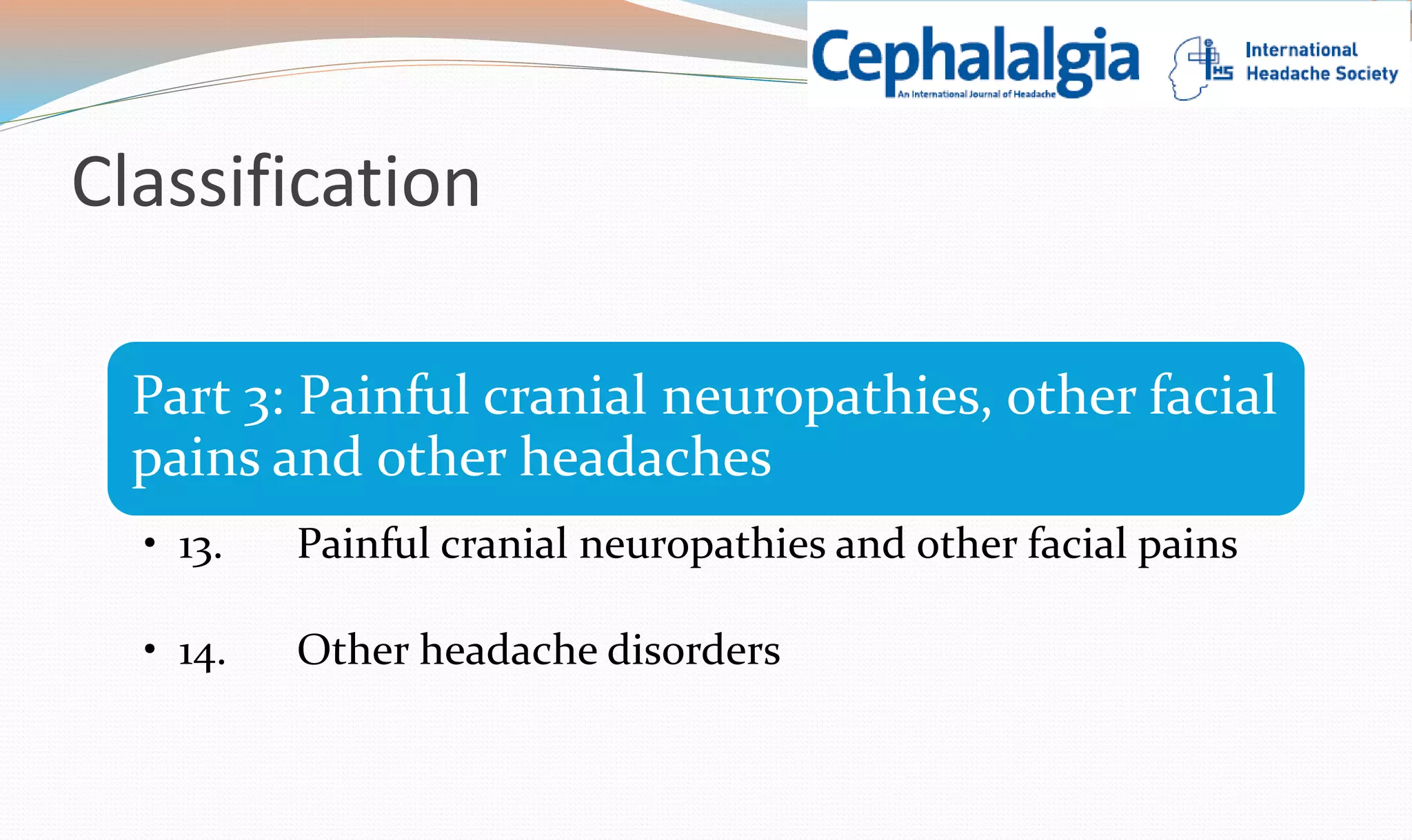
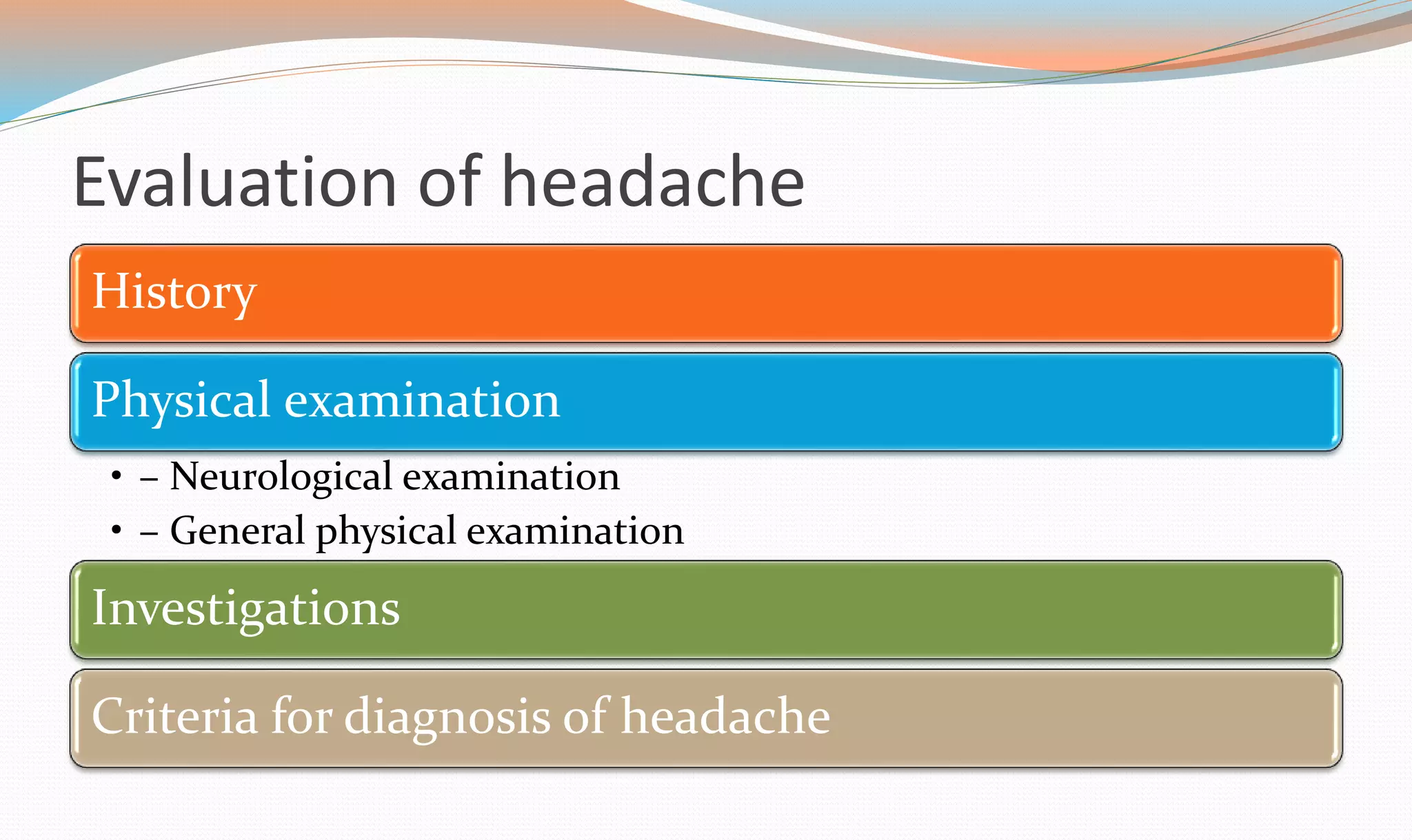
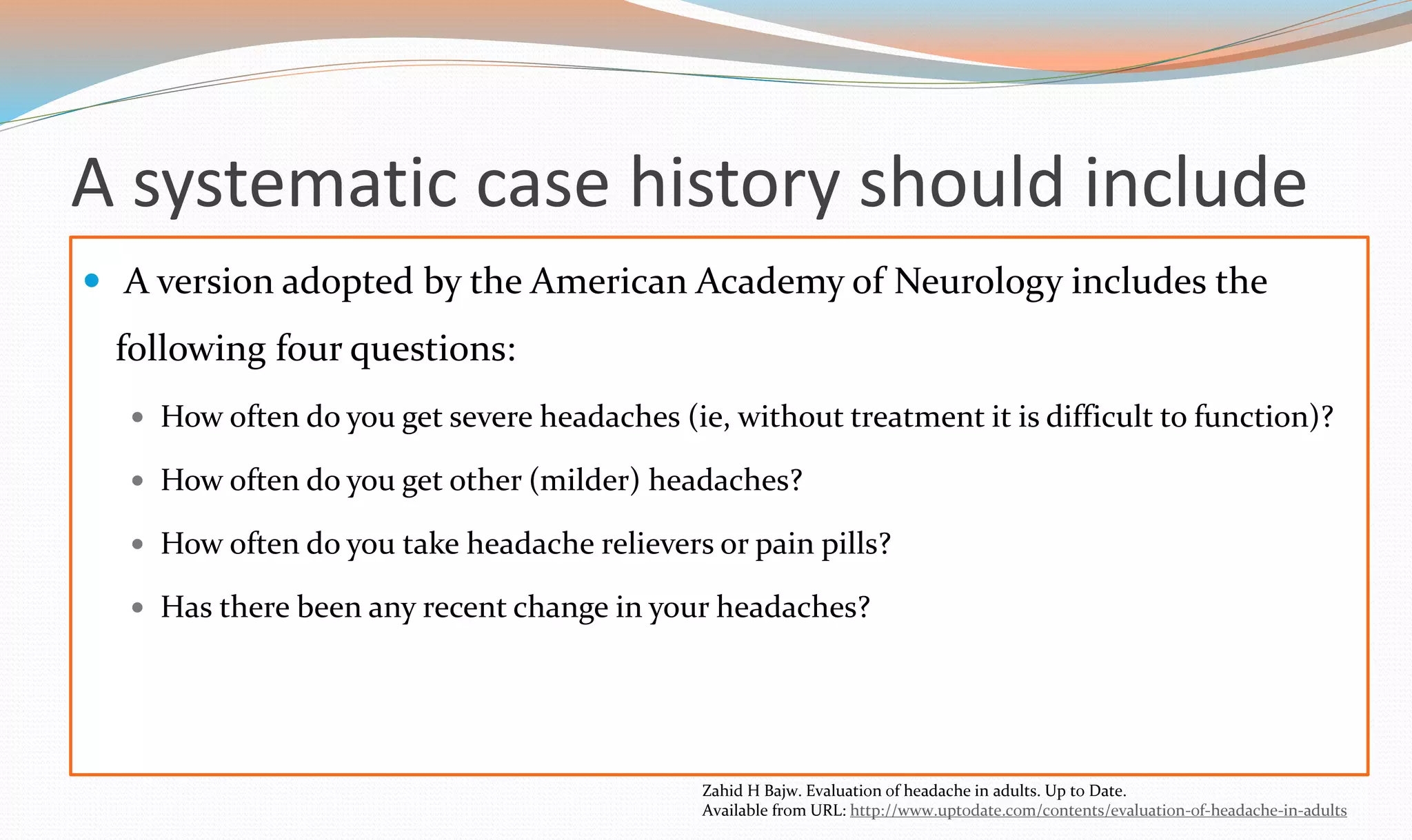
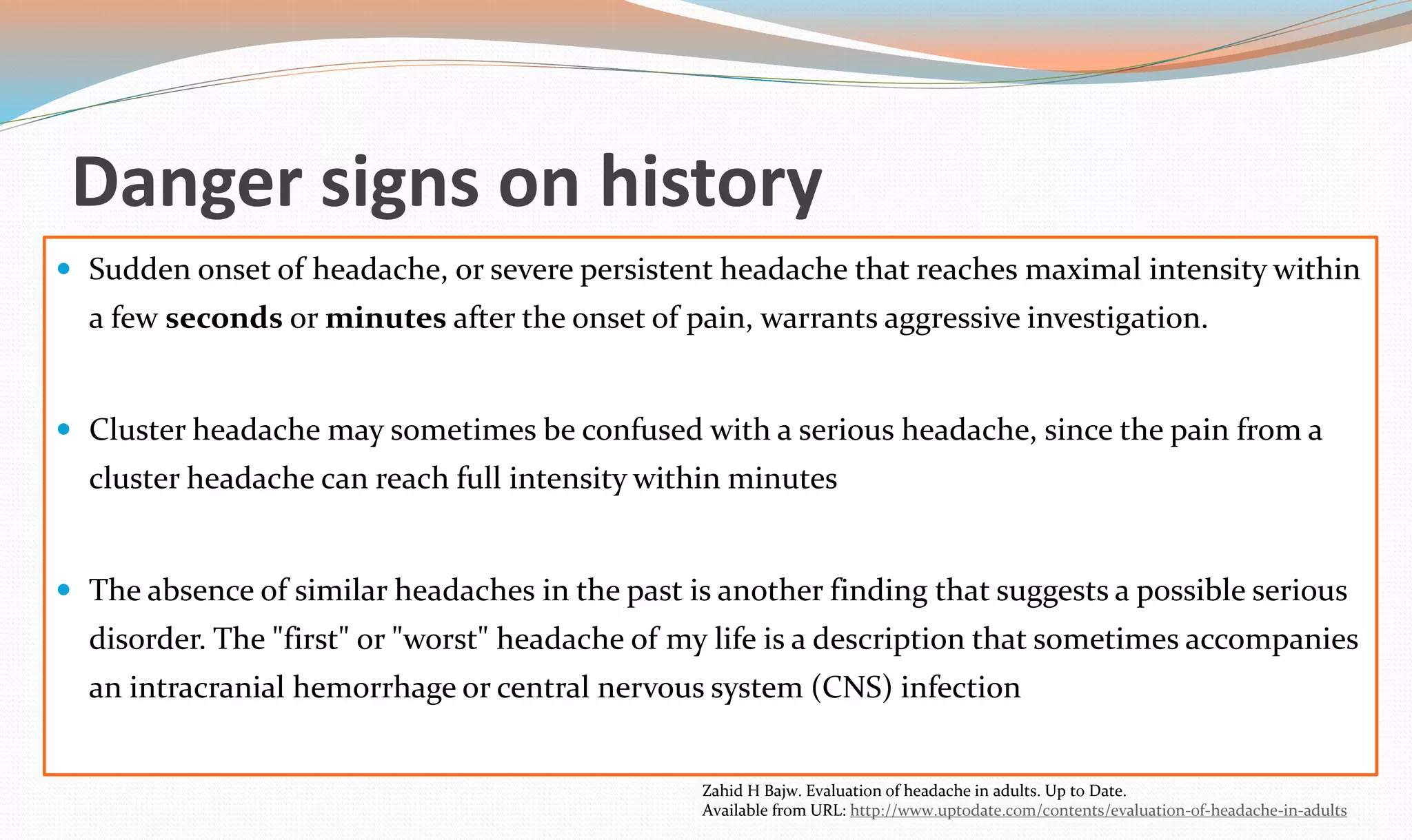
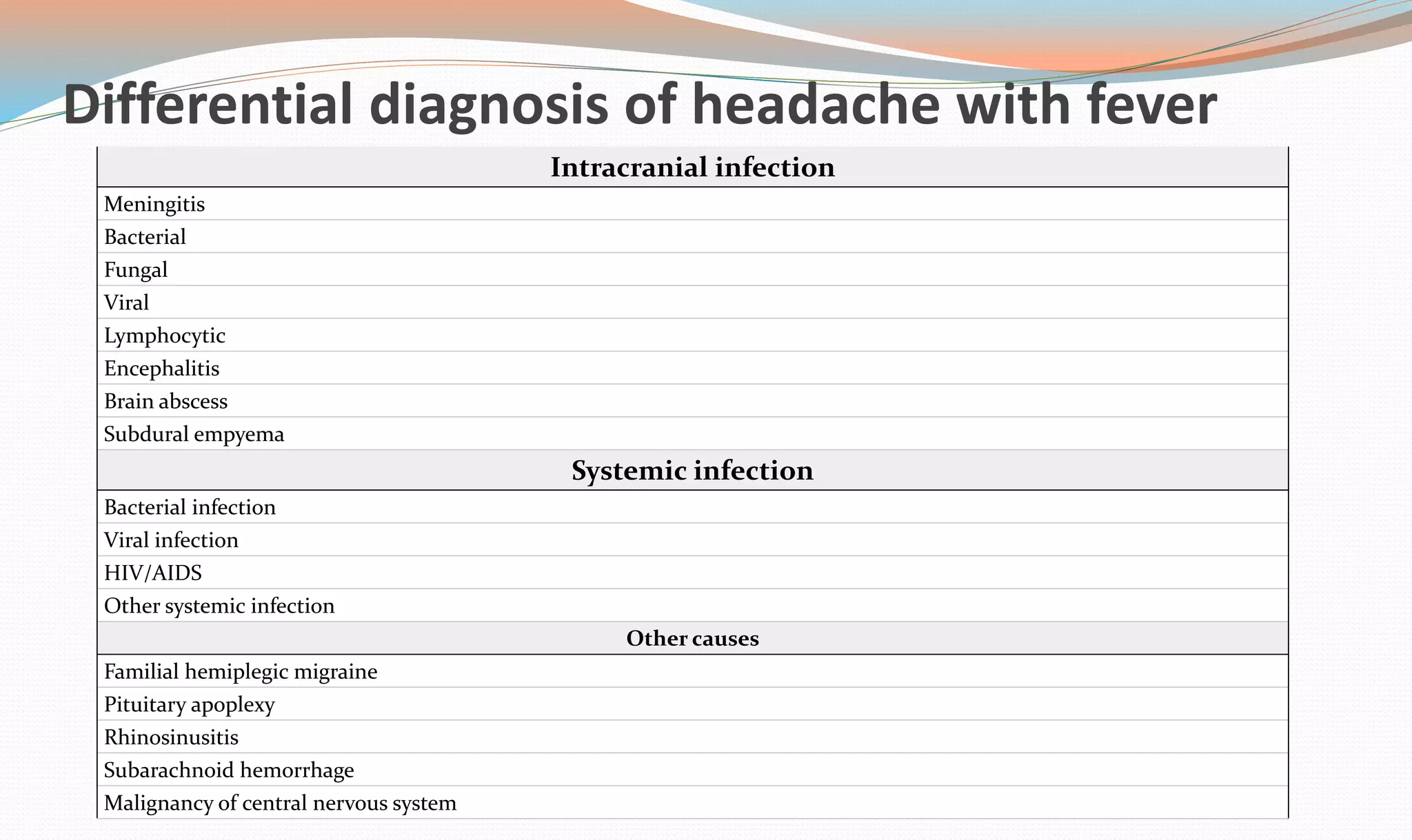
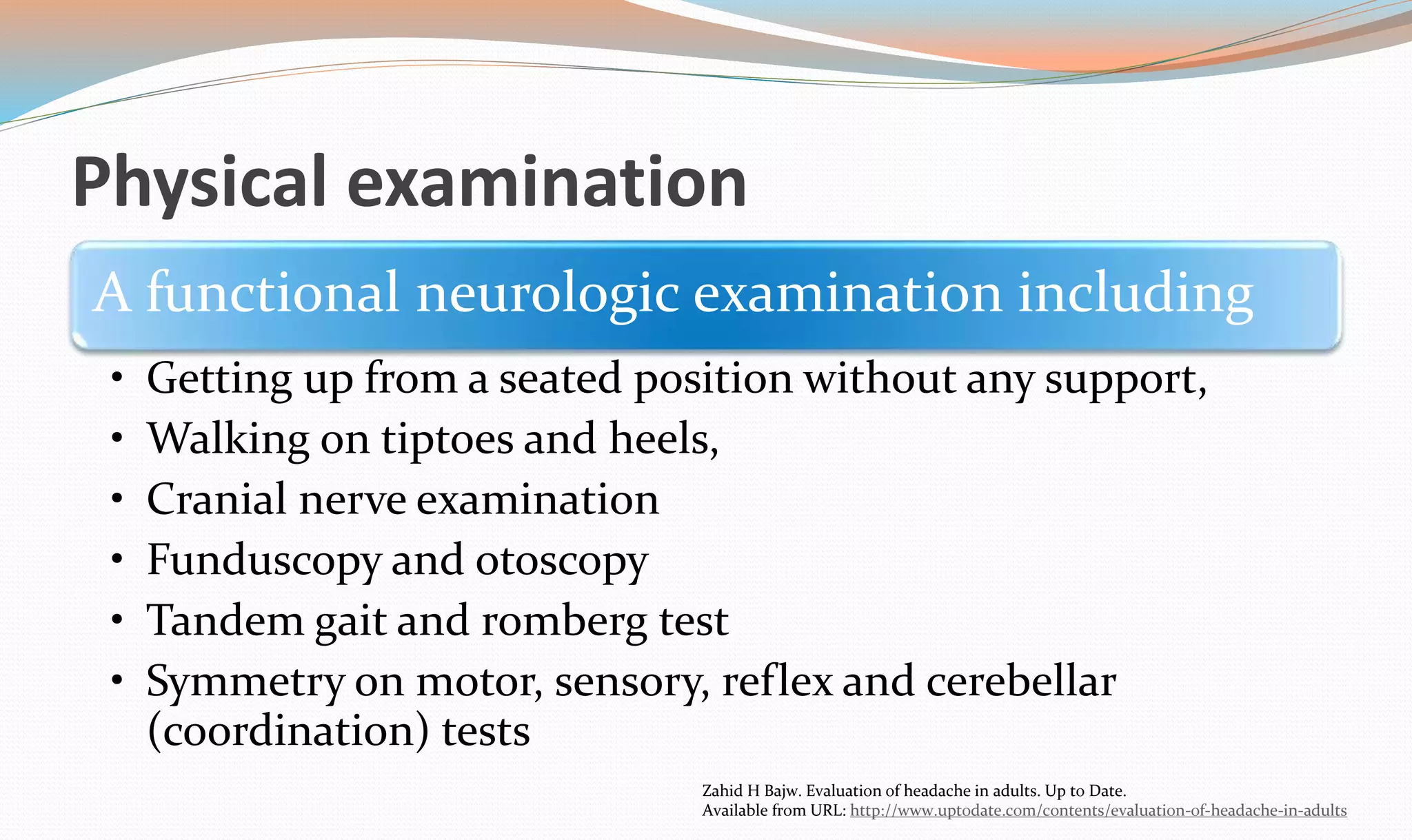
This document discusses headache disorders and their evaluation and classification. It notes that headaches are among the most common neurological disorders, affecting around 47% of adults annually. The most common types of benign headaches are migraine, tension-type, and cluster headaches. A thorough patient history is the most important part of the evaluation, to help identify headache type and risk factors for underlying conditions. Physical examination may include neurological and general examination, with attention to danger signs in the history that suggest further investigation is needed.












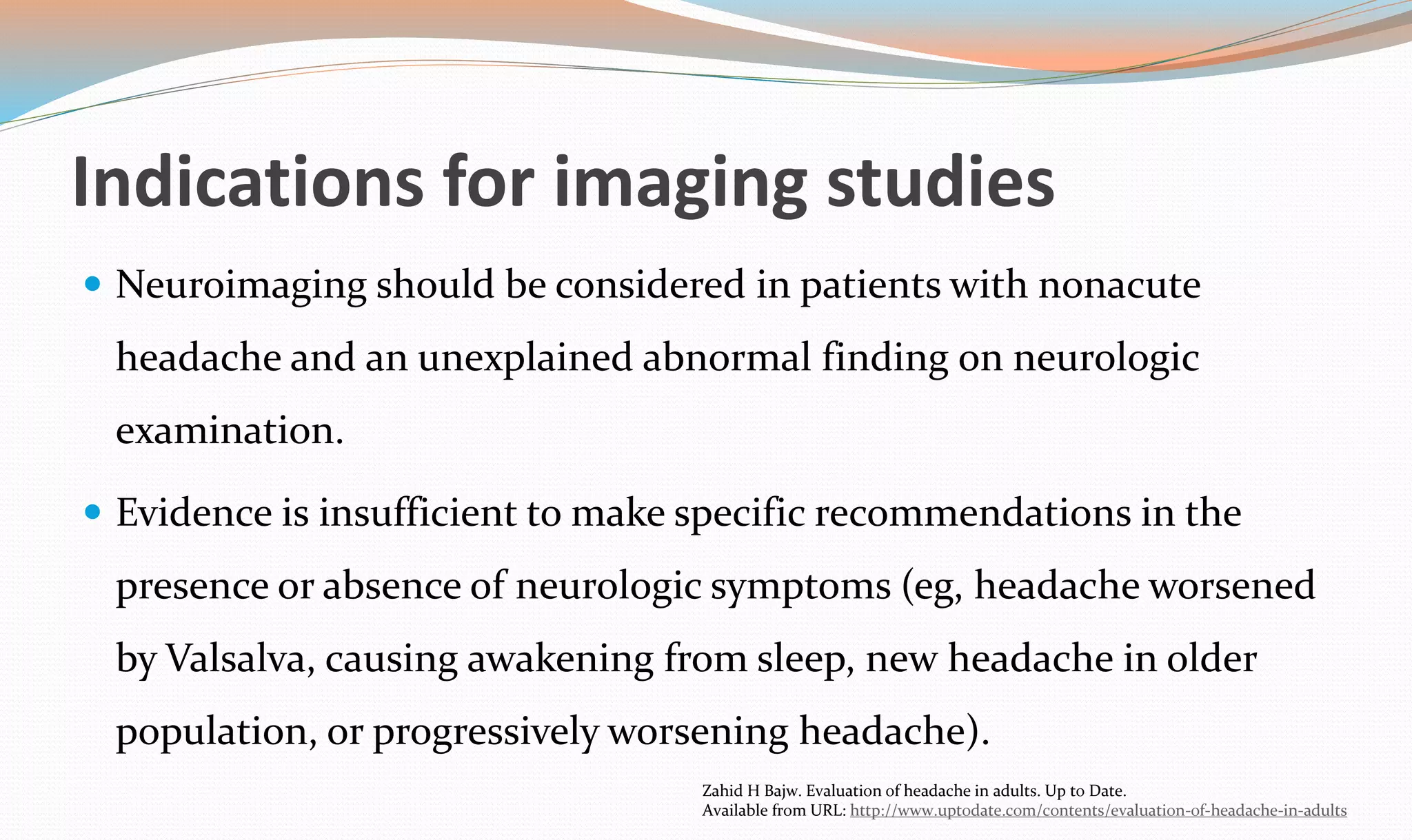









![Neuroimaging
Neuroimaging studies (eg, computed tomography [CT] or magnetic resonance
imaging [MRI]) may detect a variety of disorders that cause secondary
headache, including:
Congenital malformations
Hydrocephalus
Cranial infections and their sequelae
Trauma and its sequelae
Neoplasms
Vascular disorders (such as arteriovenous malformations)
Daniel J Bonthius. Approach to the child with headache. Up To Date.
Available from URL: www.uptodate.com.](https://image.slidesharecdn.com/headache-141021042914-conversion-gate02/75/Headache-39-2048.jpg)