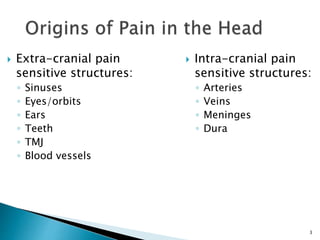
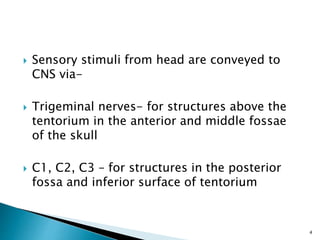
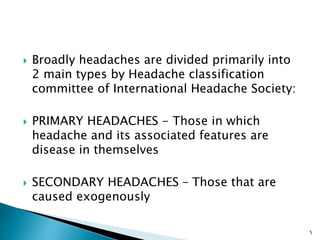
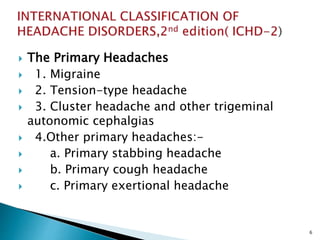
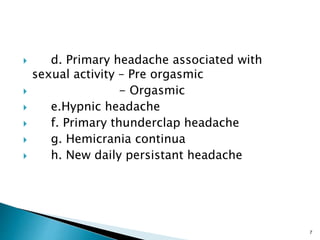
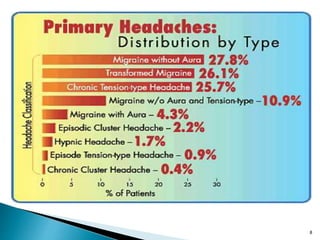
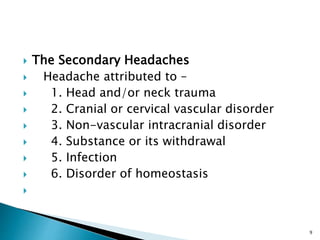
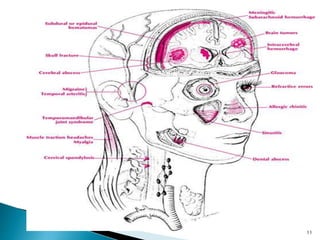
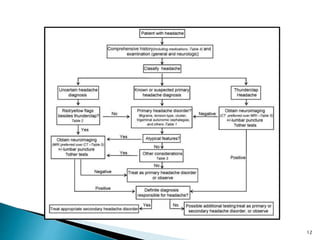
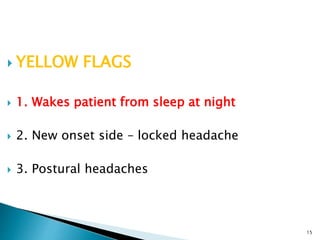
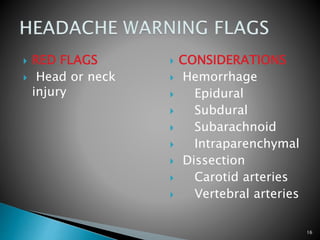
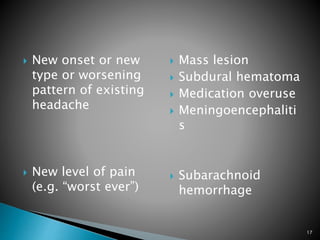
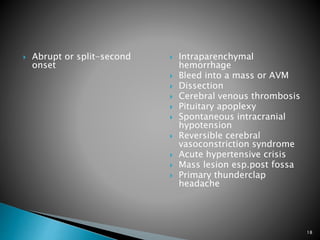
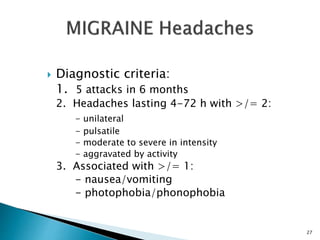
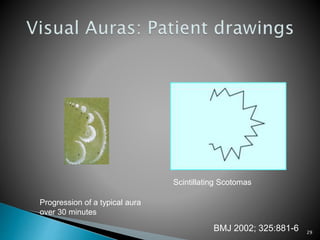
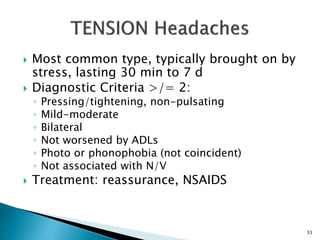
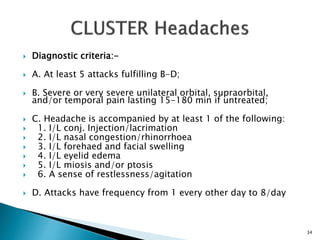
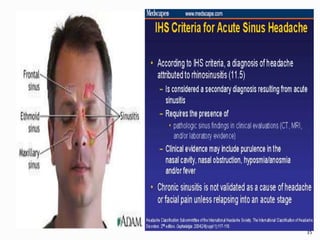
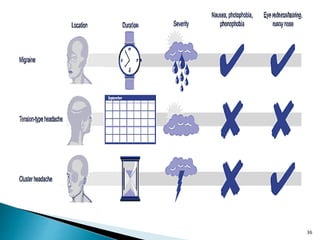
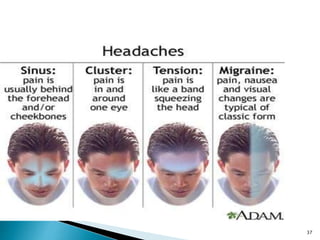
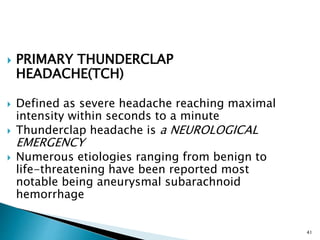
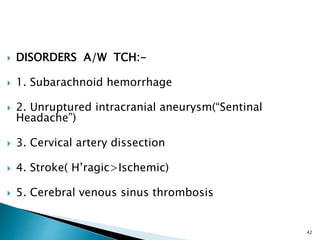
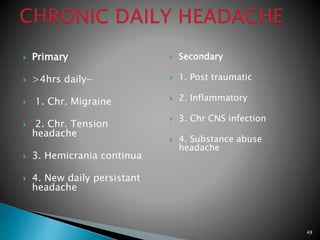
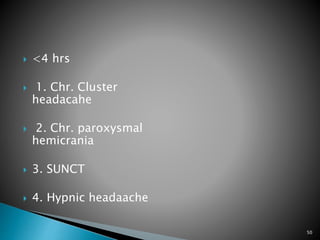
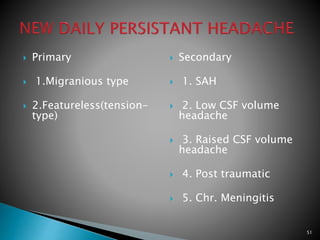
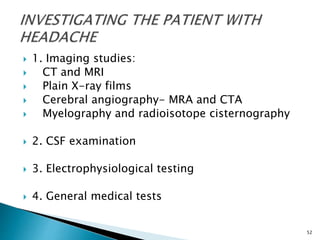
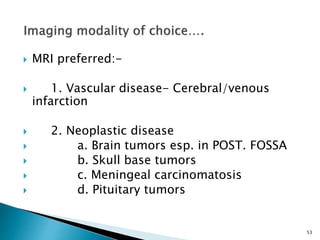
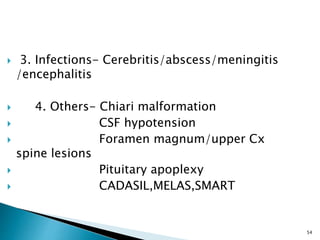
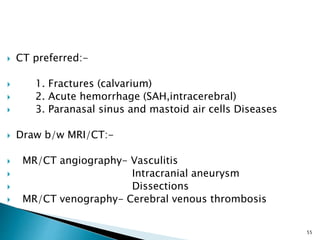
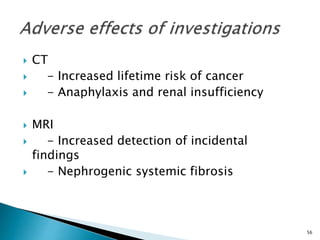
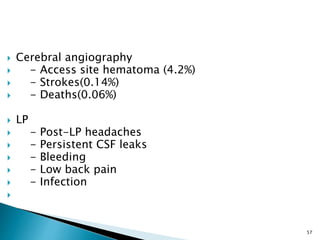
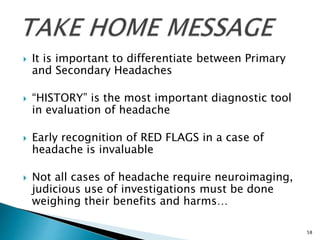
This document discusses the approach to evaluating and diagnosing patients presenting with headache. It begins by distinguishing between primary and secondary headaches. Primary headaches include migraine, tension-type headache, and cluster headache, while secondary headaches are caused by underlying conditions like head trauma, vascular disorders, or infections. The document outlines diagnostic criteria for common headache types and recommends investigations and treatment approaches based on the presence of "red flags" or alarming symptoms.