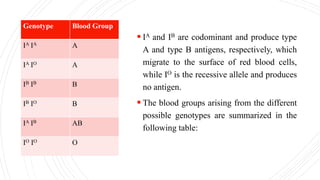
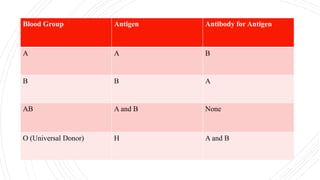
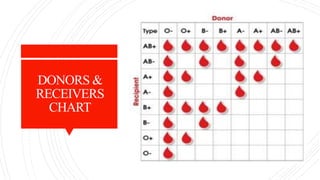
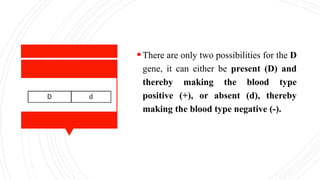
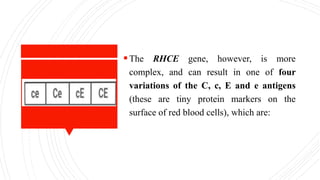
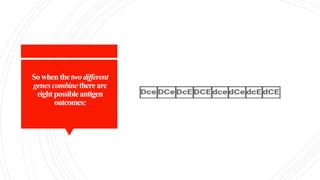
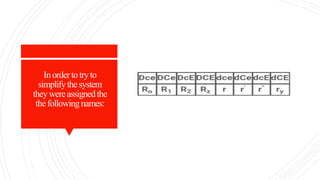
This document discusses multiple alleles and the ABO blood grouping system. It begins by defining alleles and describing how multiple alleles can exist for a single gene. It then focuses on explaining the ABO blood grouping system, which is controlled by three alleles (IA, IB, IO) that determine the A, B, and O blood types. The document outlines the antigens and antibodies present in each blood type, as well as rare blood types like Bombay and Rhnull. It also discusses cross-matching for transfusions and potential sources of errors or mutations in blood group transmission.