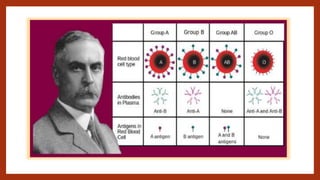
This document discusses blood grouping and typing systems including ABO and Rh. It provides details on the antigens and antibodies involved, the biochemical basis, and clinical significance for transfusion and disease. The key points are:
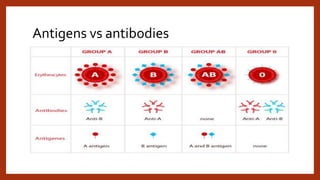
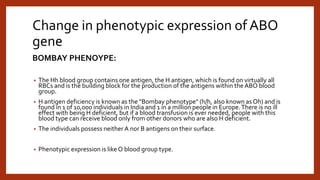
1) The ABO system is the most important for transfusion due to naturally occurring antibodies. Incompatible blood can cause hemolysis.
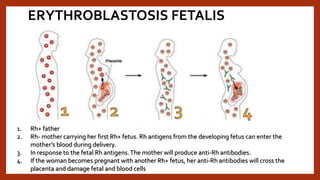
2) The Rh system involves the D antigen which is immunogenic; incompatibility can cause hemolytic disease of the newborn.
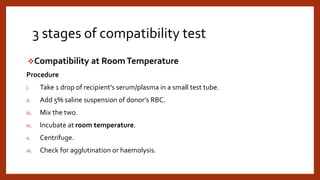
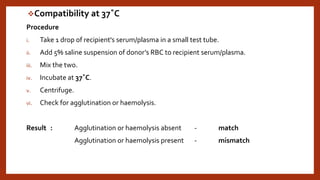
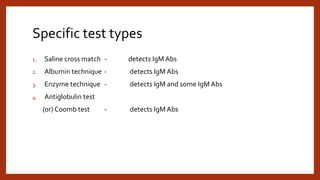
3) Cross-matching tests for compatibility between donor and recipient blood to prevent transfusion reactions from antibodies.
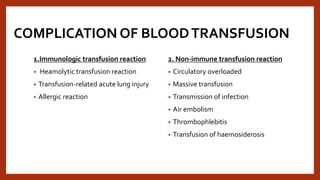
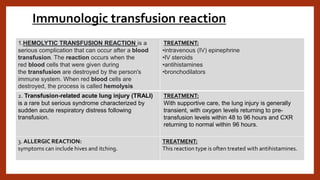
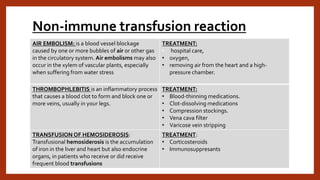
![Non-immune transfusion reaction
TRANSFUSION ASSOCIATED CIRCULATORY
OVERLOAD : includes any four of the following
occurring within 6 h of a BT[3] - acute respiratory
distress, tachycardia, increased blood pressure (BP),
acute or worsening pulmonary edema and evidence of
a positive fluid balance.
TREATMENT:
Move the patient into a sitting position and
administer oxygen to facilitate breathing.The most
specific treatment is discontinuing the transfusion and
removing the excessive fluid.
MASSIVETRANSFUSION is traditionally defined as
transfusion of 10 units of packed red blood cells
(PRBCs) within a 24 hour period.
TREATMENT:
MassiveTransfusion Protocol” (MTP) refers to rapid
administration of large amounts of blood products (at
least 6 units of PRBC) in fixed ratios (usually 1:1:1) for
the management of hemorrhagic shock. Only a subset
of patients with “massive transfusion” will receive
a massive transfusion protocol.
TRANSFUSION-TRANSMITTED INFECTIONS (TTIS)
are infections resulting from the introduction of a
pathogen into a person through blood transfusion. A
wide variety of organisms, including bacteria, viruses,
prions, and parasites can be transmitted through
blood transfusions.
TREATMENT:
• donor selection
• the screening of donations
• specific processing
• quarantine of plasma
• bacterial culturing
• post-donation and post-transfusion notification](https://image.slidesharecdn.com/bloodgrouping-230627180238-fd499aed/85/Blood-Grouping-pptx-44-320.jpg)