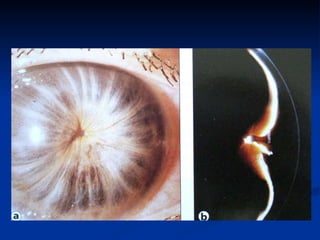
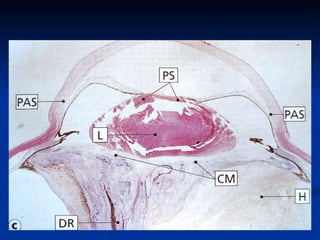
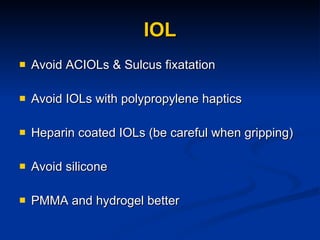
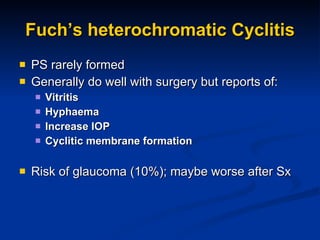
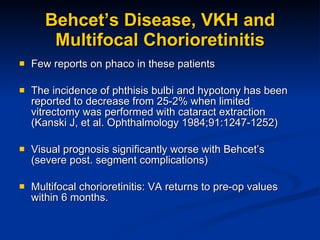
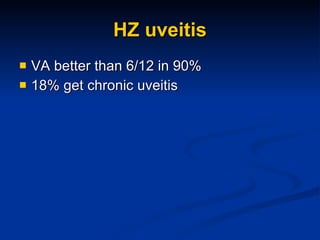
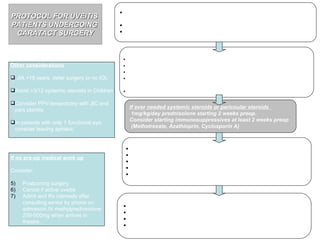
The document discusses guidelines for performing cataract surgery on patients with uveitis. It outlines several challenges including pre-operative and post-operative inflammation control and technical difficulties during surgery. The guidelines recommend thorough pre-operative control of inflammation, careful surgical techniques such as phacoemulsification instead of extracapsular extraction, and strict post-operative anti-inflammatory treatment to minimize complications for these high-risk patients. Special considerations are discussed for different types of uveitis.