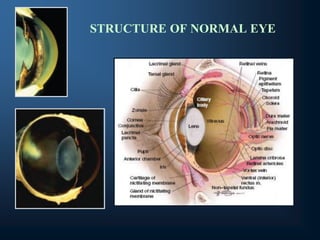
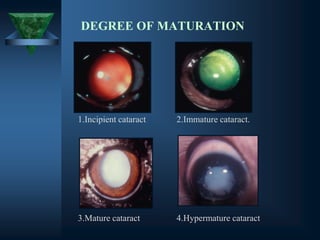
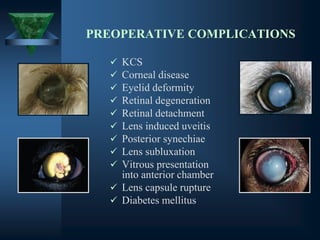
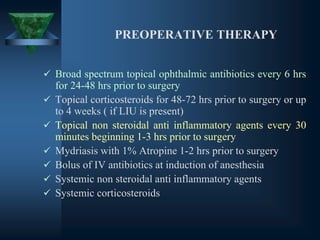
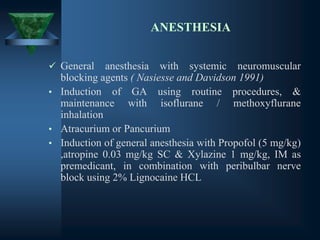
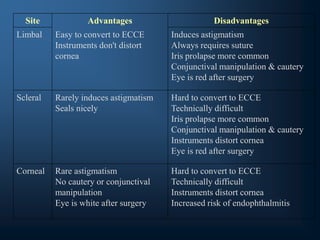
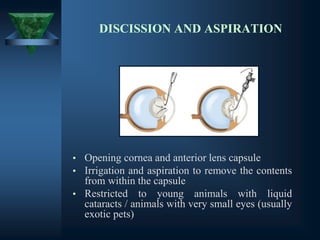
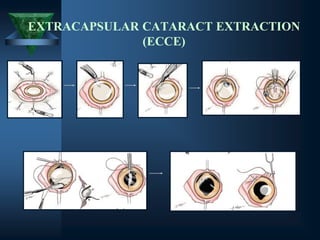
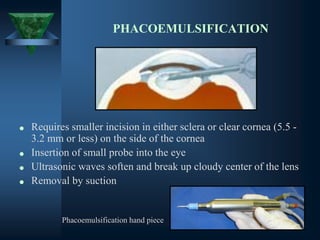
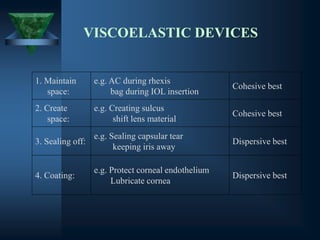
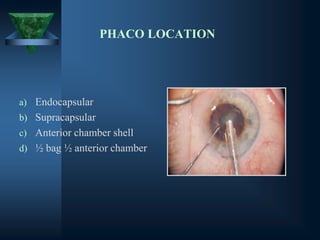
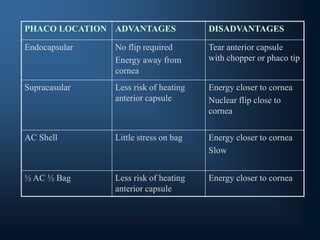
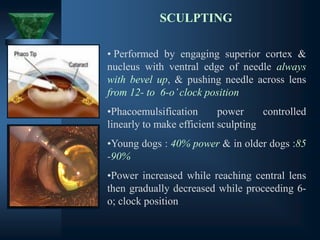
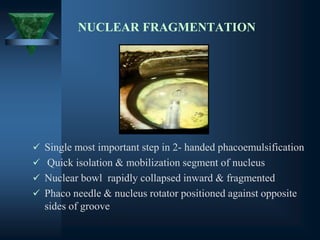
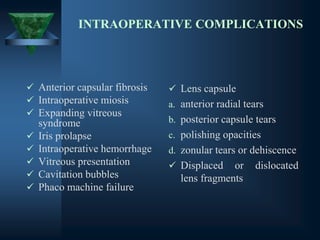
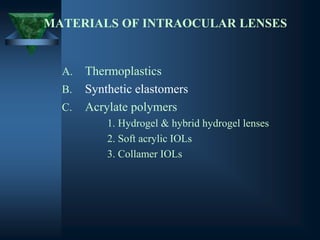
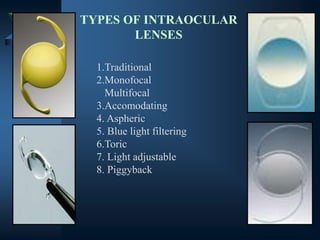
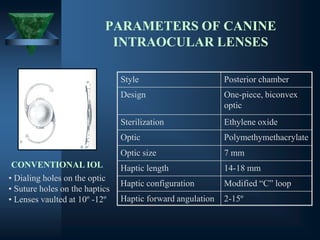
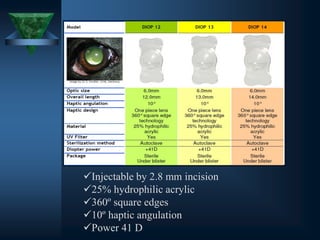
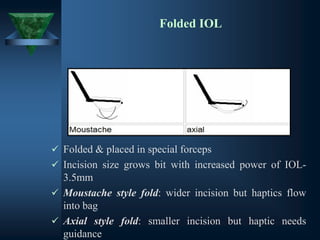
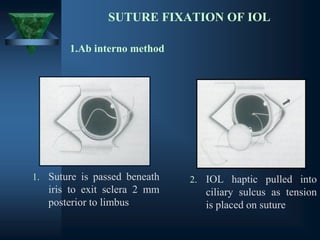
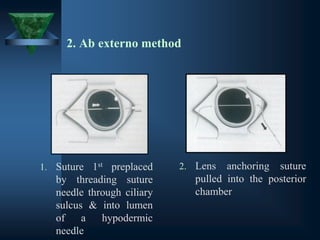
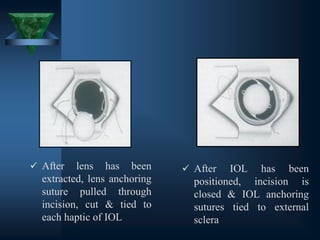
This document provides information on cataract surgery and intraocular lens implantation in dogs. It discusses the structure of the normal eye, different types and classifications of cataracts. It describes various surgical techniques for cataract removal including discission and aspiration, extracapsular extraction, and phacoemulsification. It also covers patient selection, pre-operative care, anesthesia, intraocular lenses, and post-operative care and complications. The goal of cataract surgery is to remove the opaque lens and restore vision through implantation of an intraocular lens.