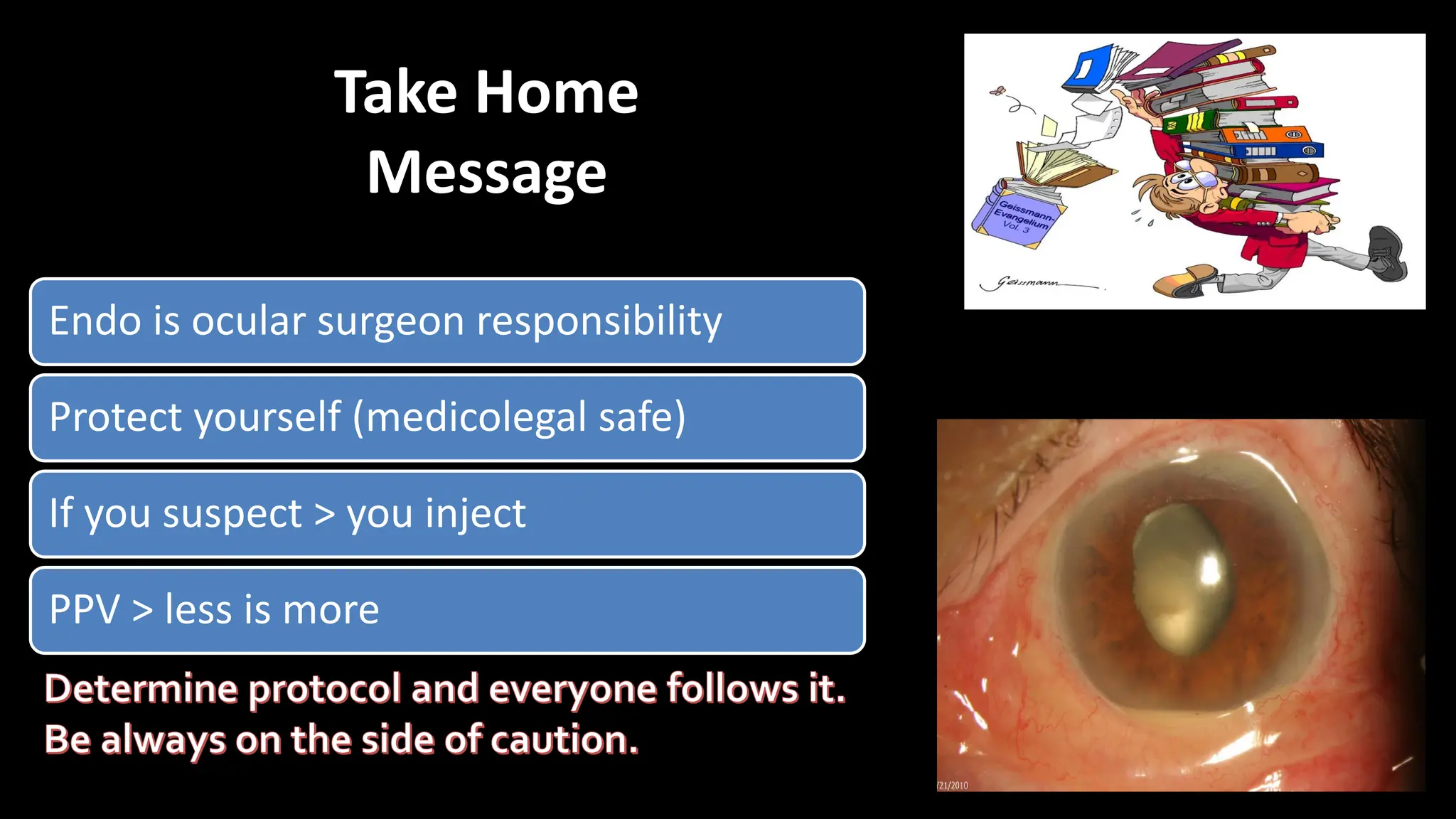
The document discusses endophthalmitis and TASS (toxic anterior segment syndrome), highlighting their causes, symptoms, and treatment options after intraocular surgery. It emphasizes the importance of proper sterile techniques and preventative measures to avoid infections, along with the management of acute inflammatory reactions. Additionally, it reviews various antibiotics and the importance of timely intervention in cases of suspected infection.