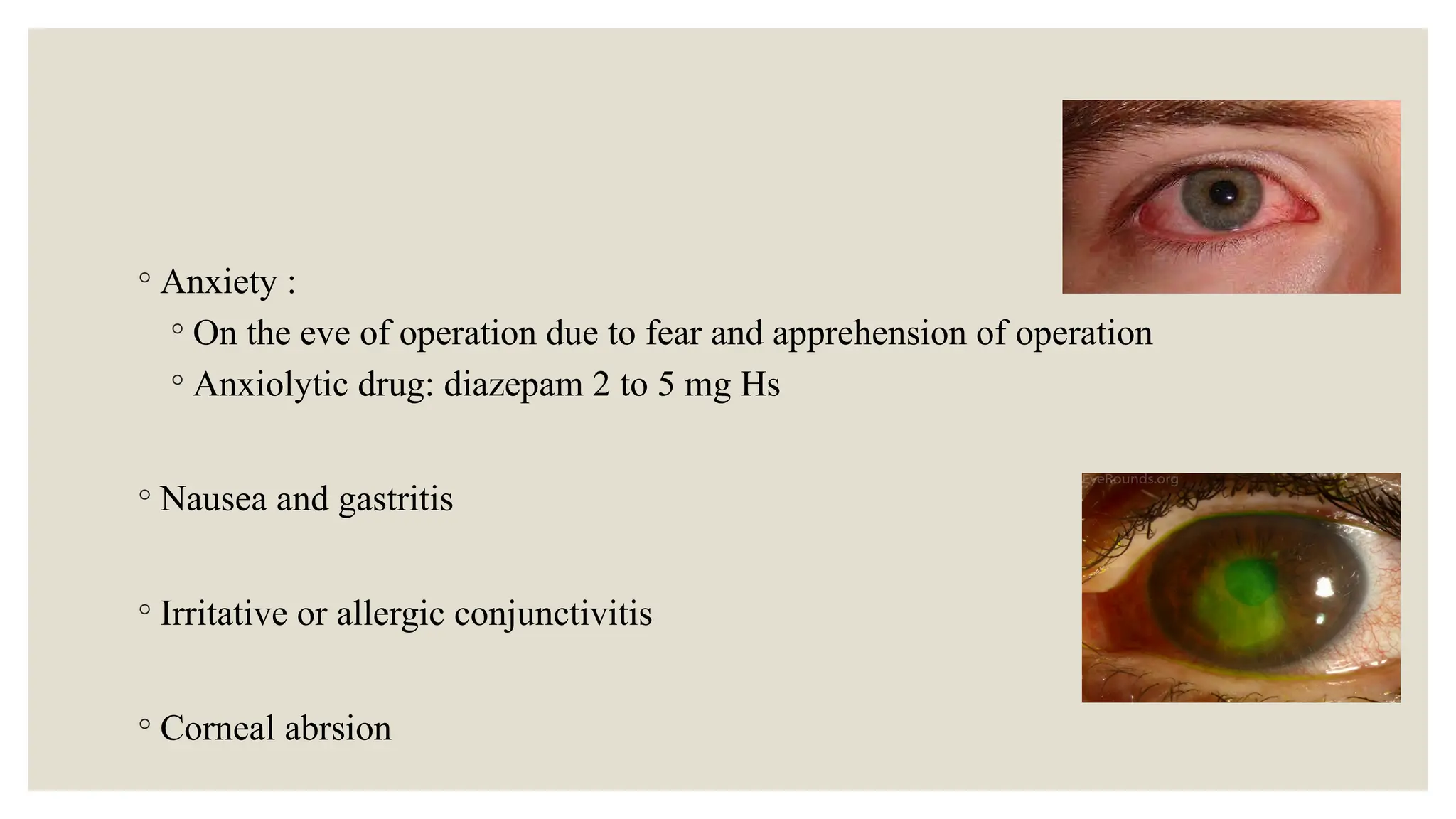
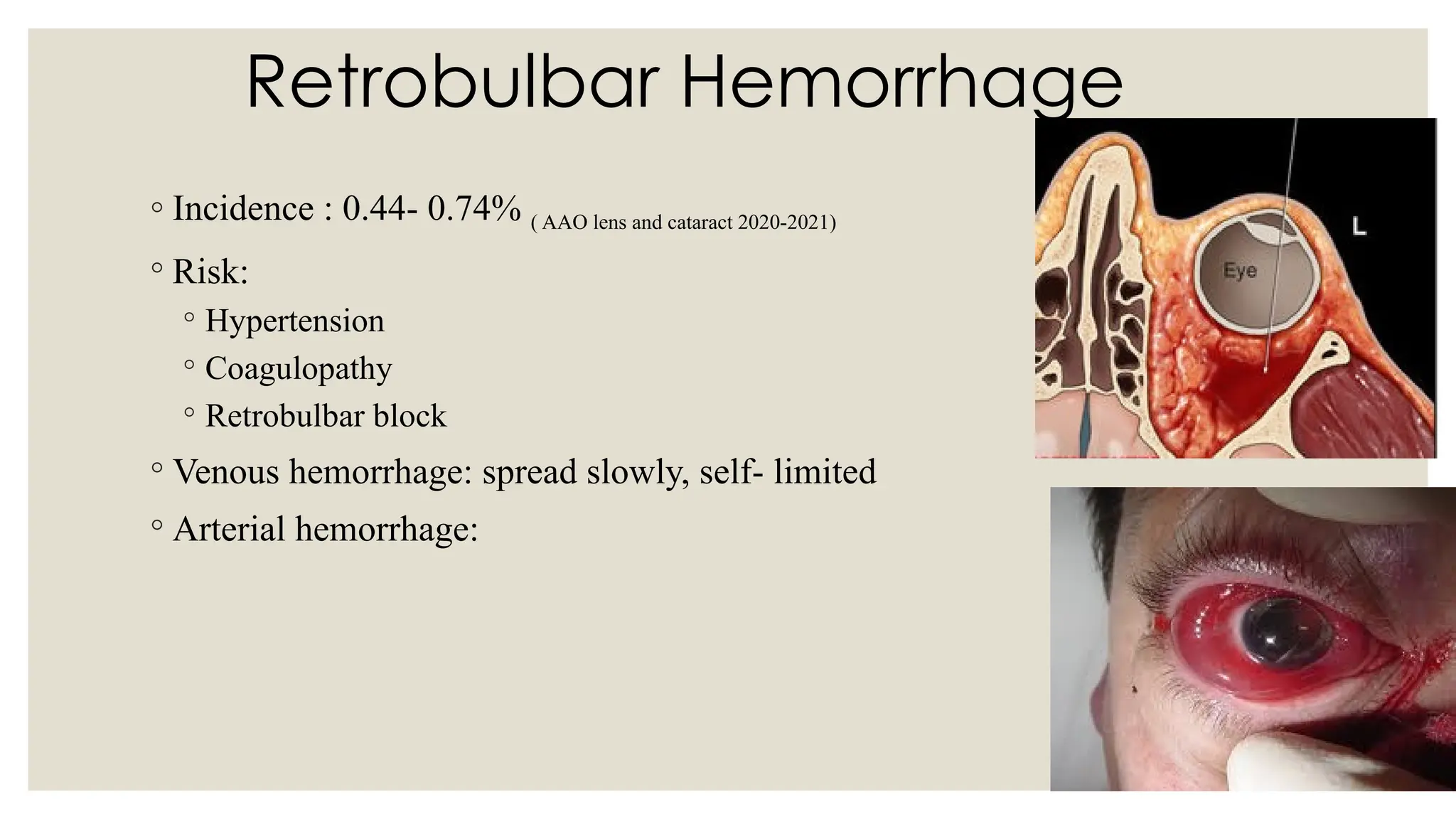
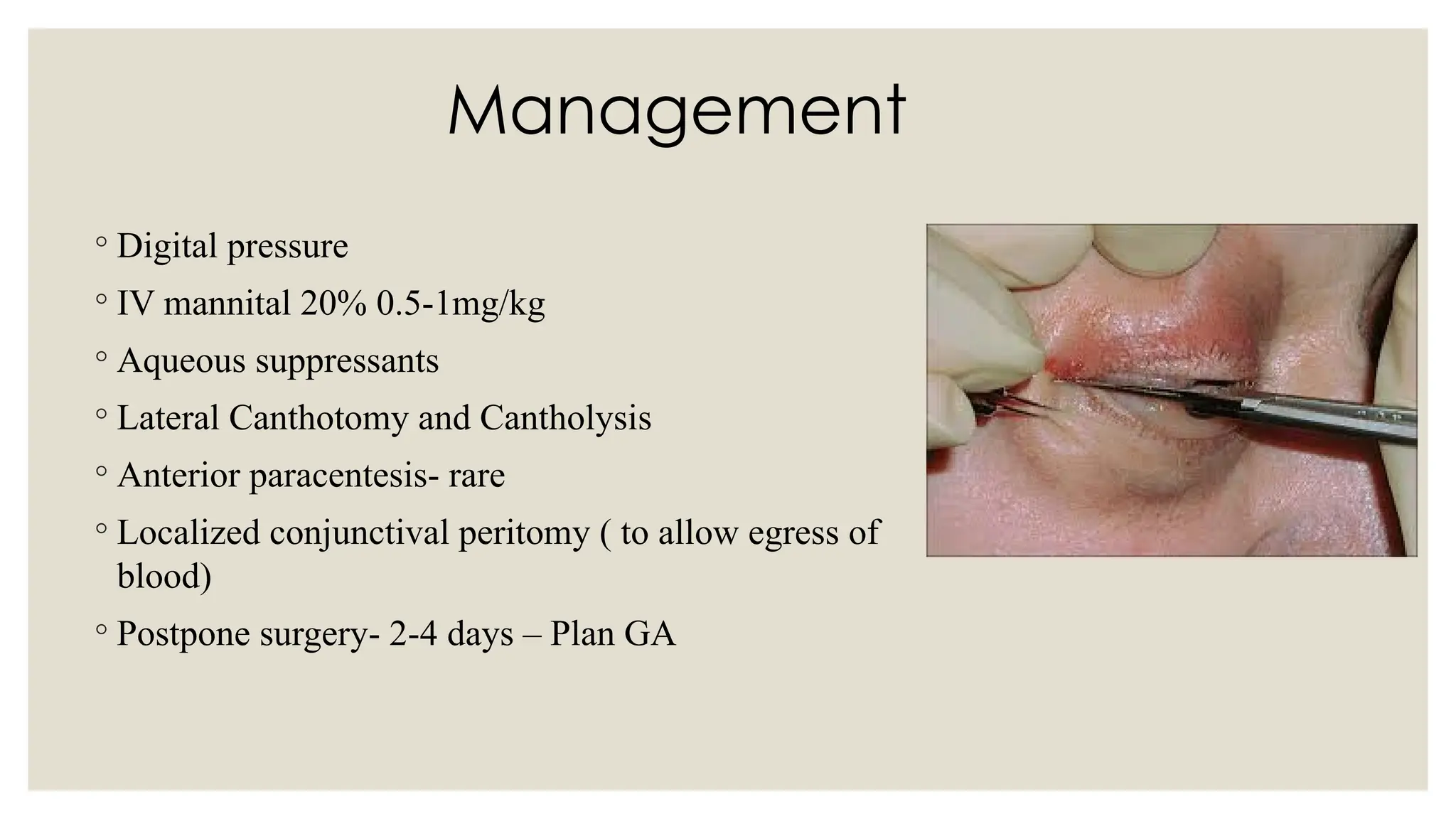
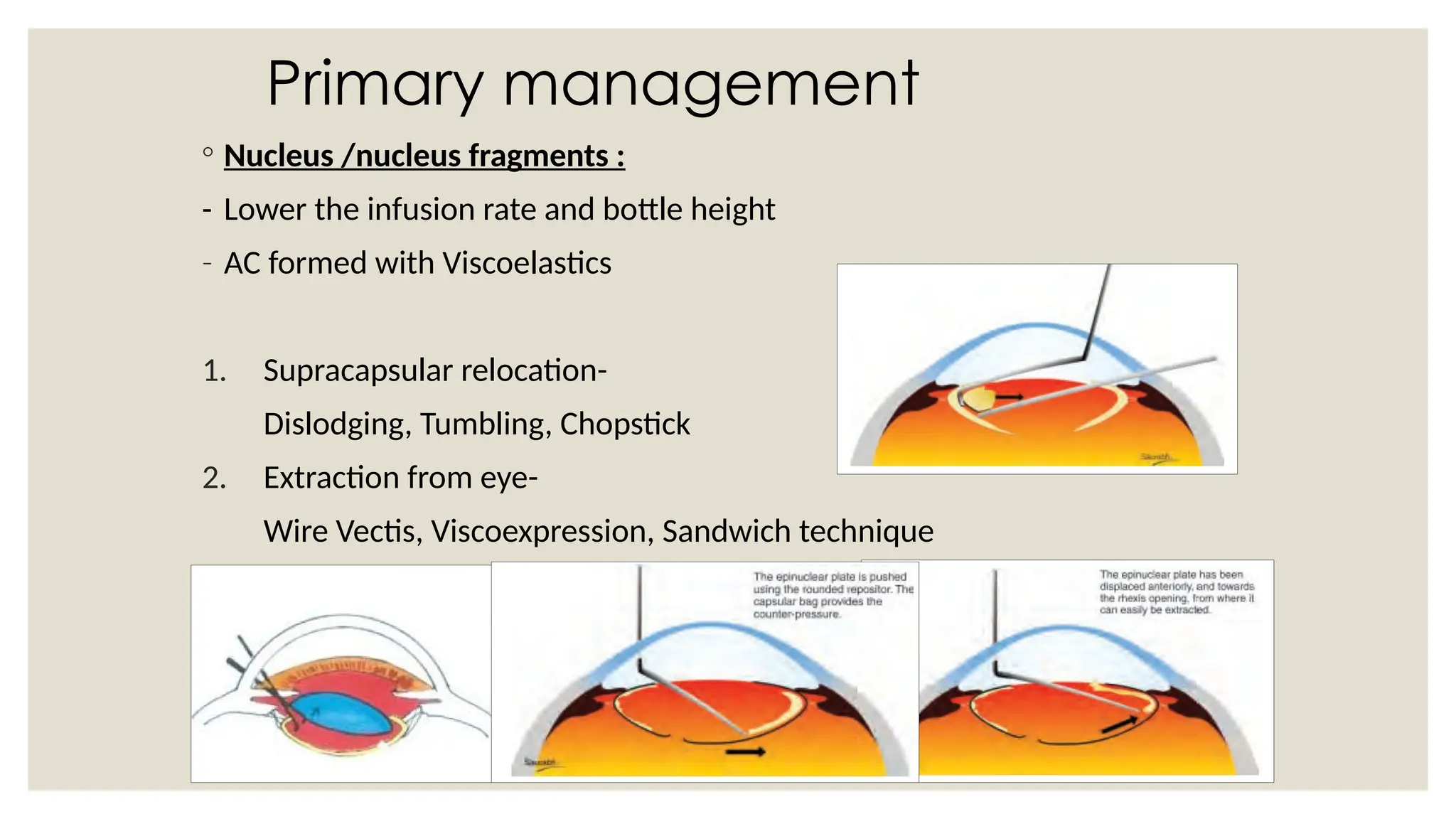
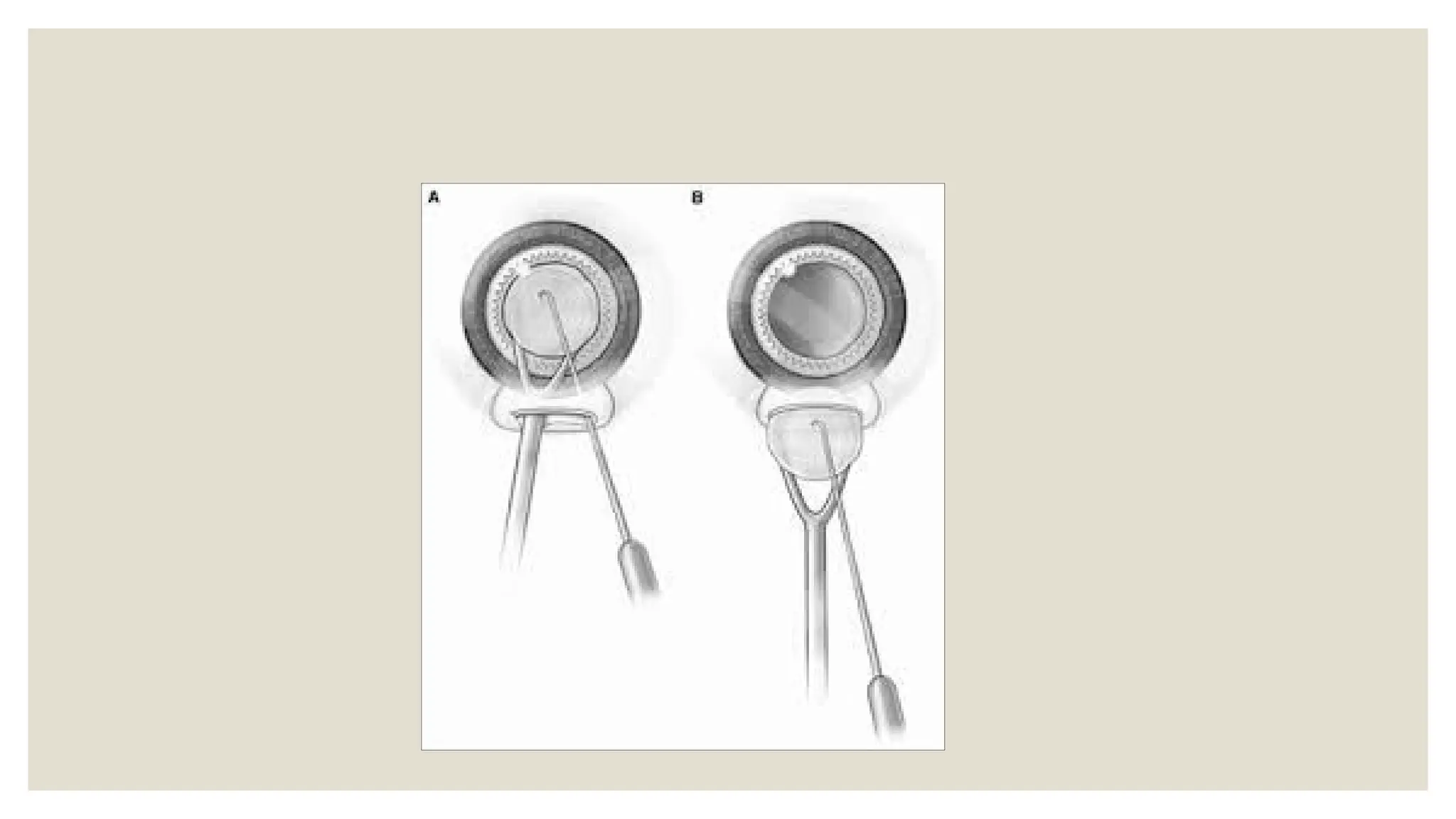
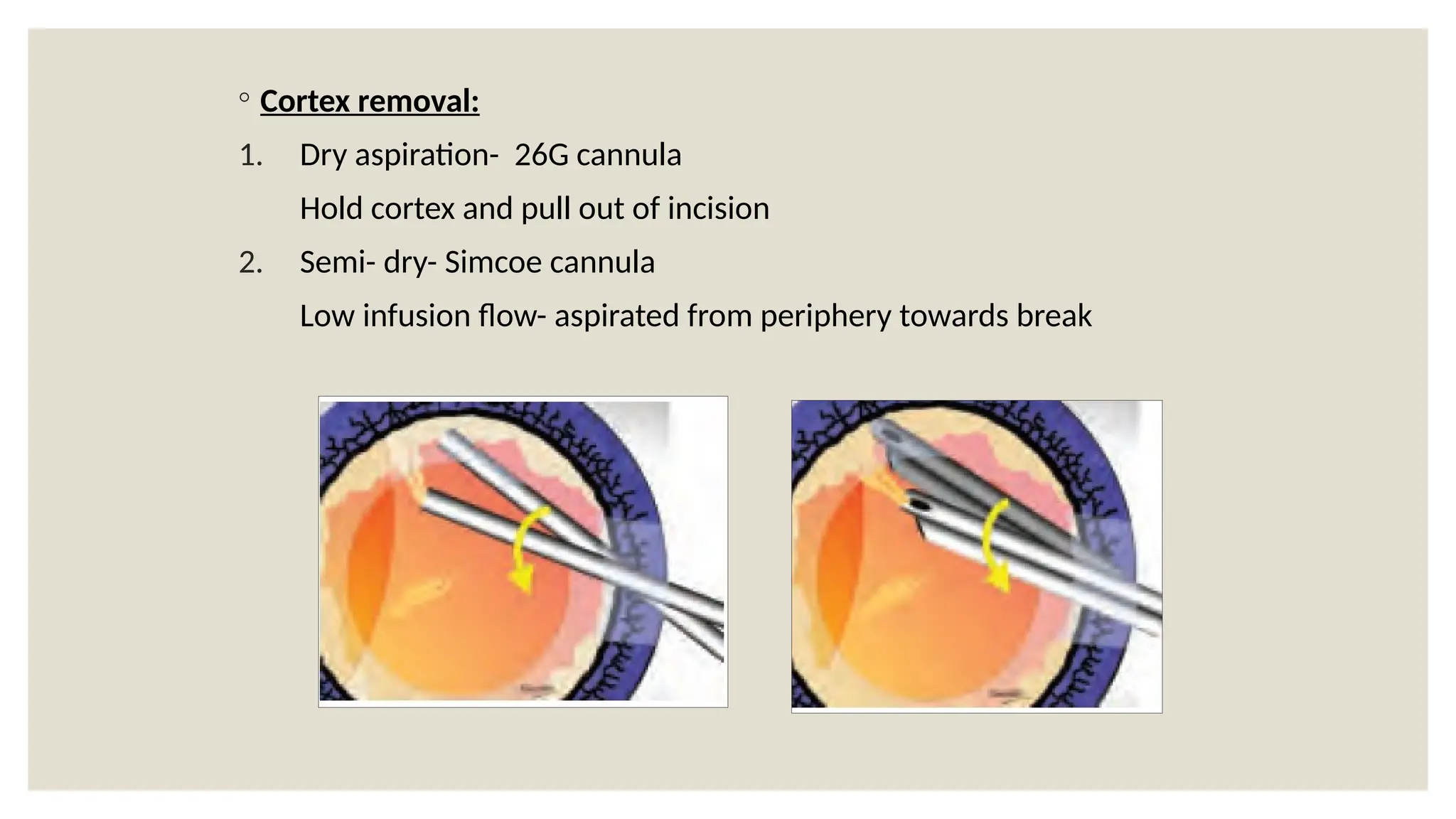
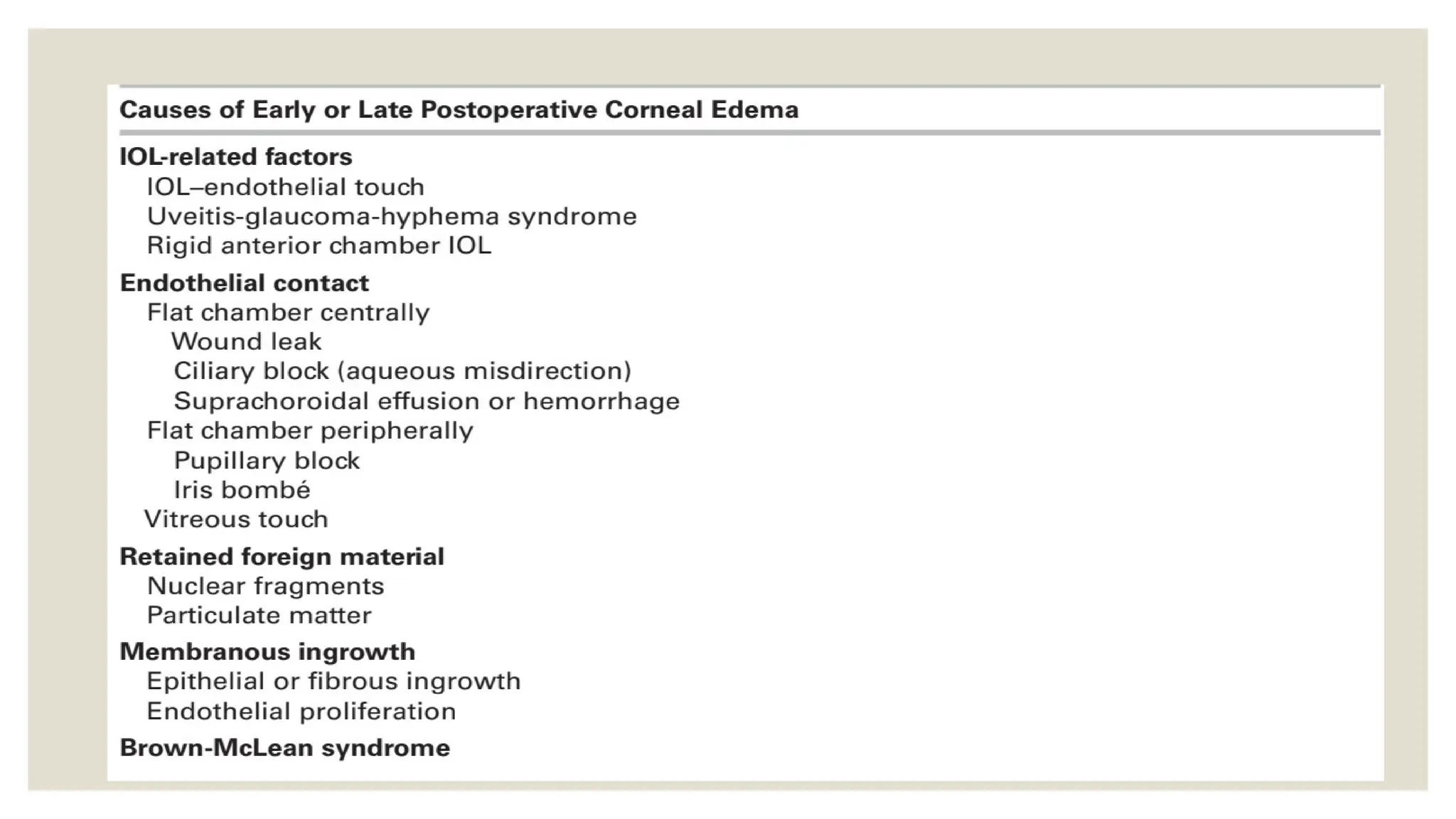
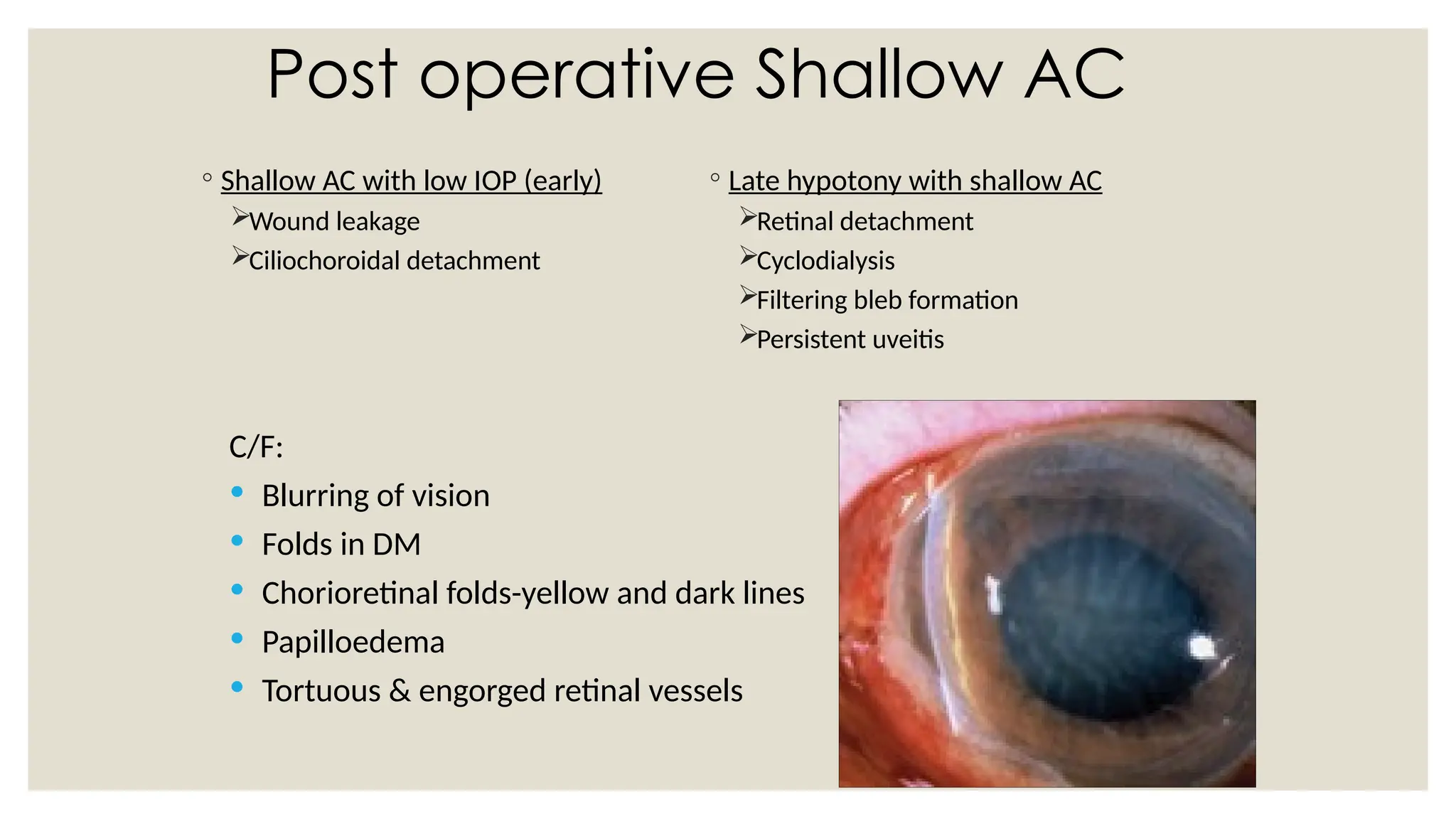
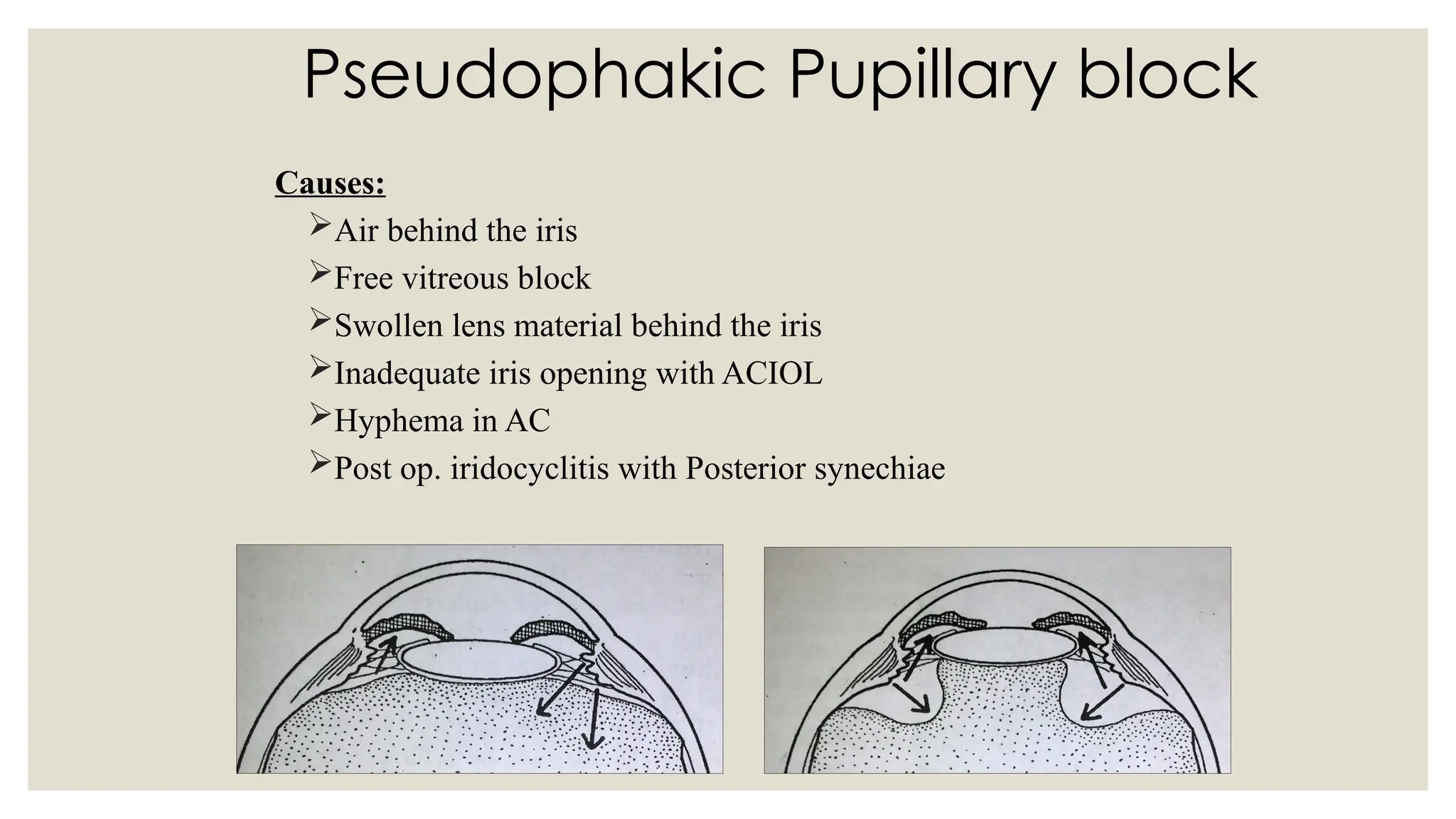
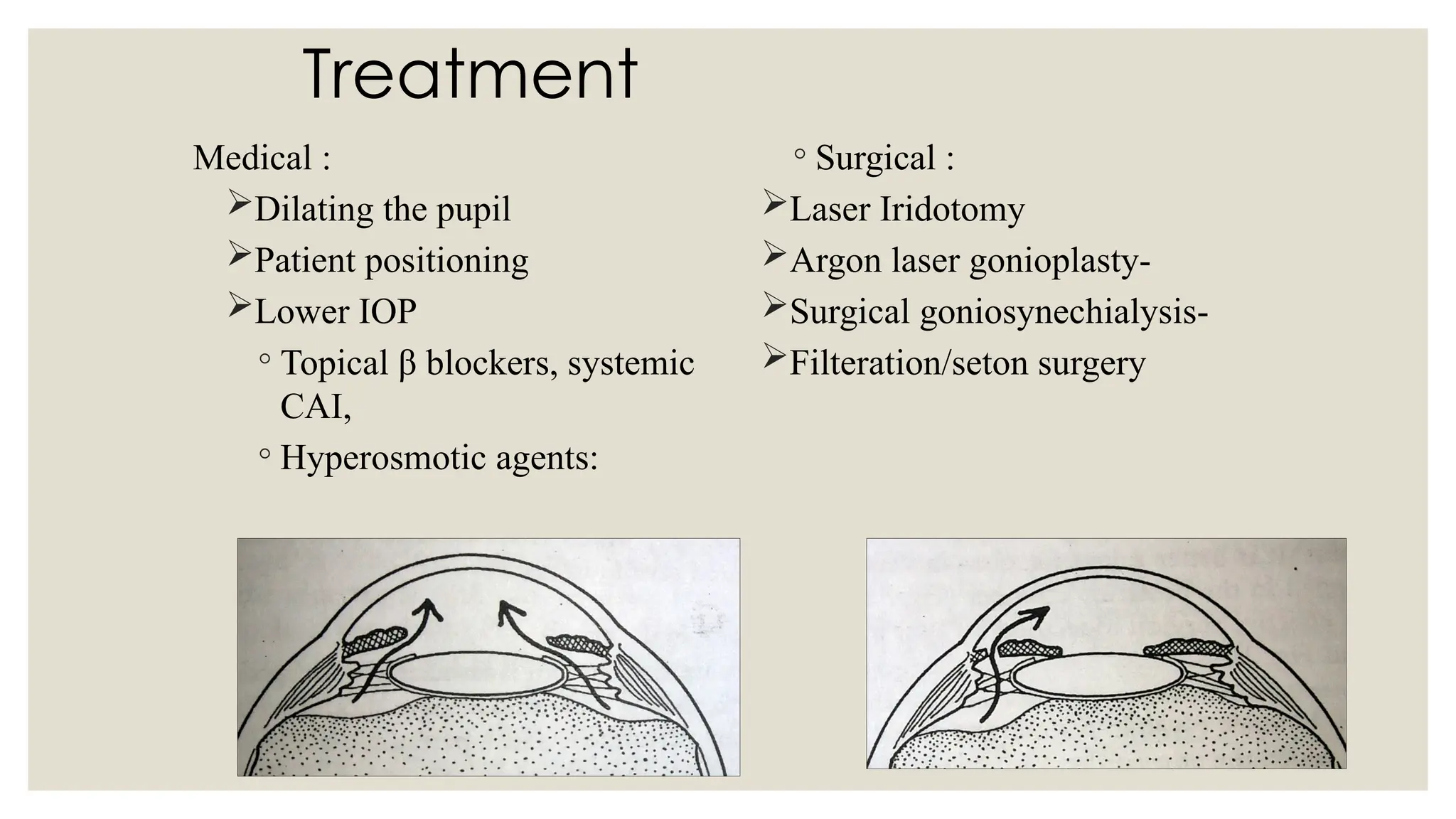
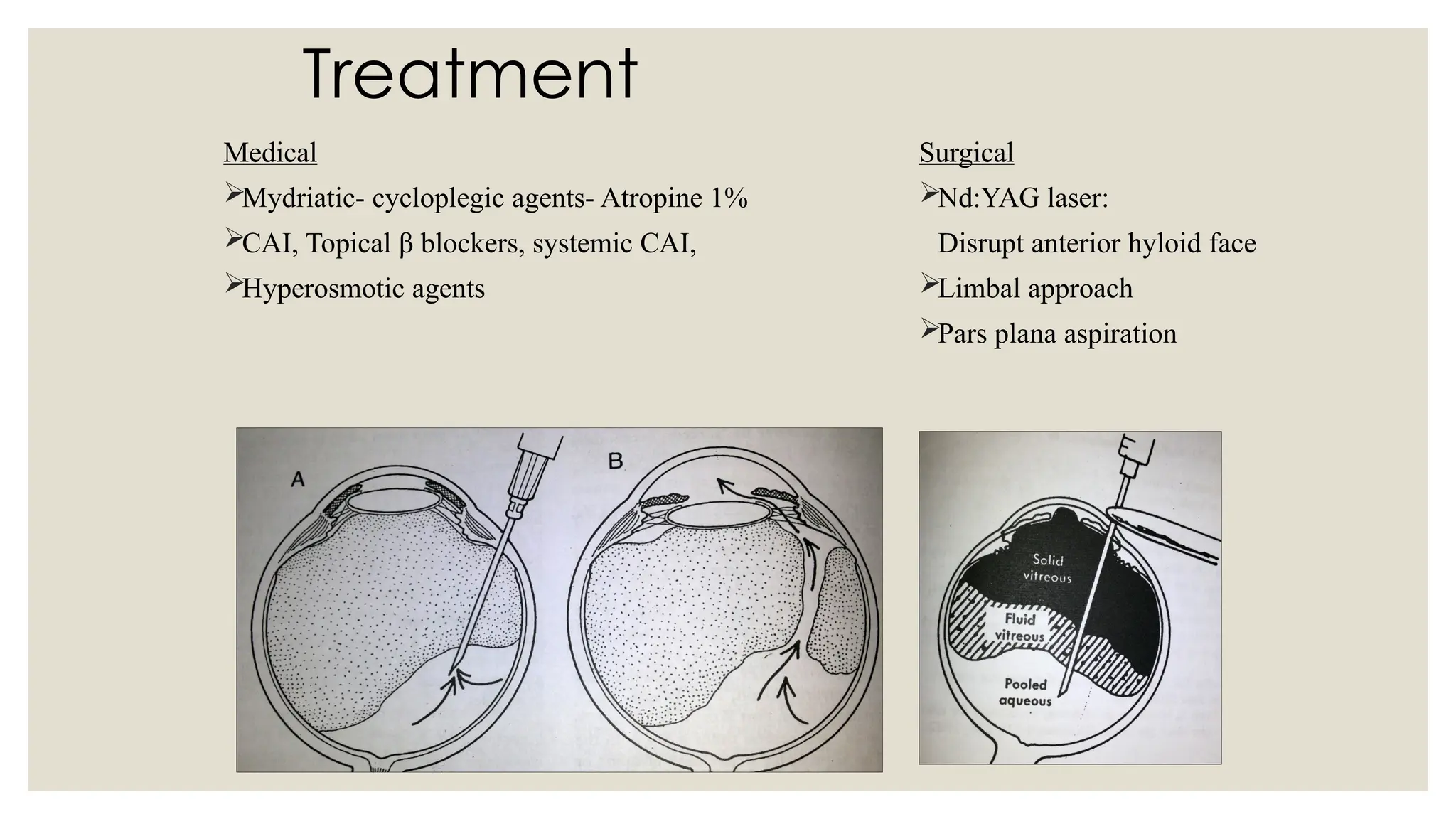
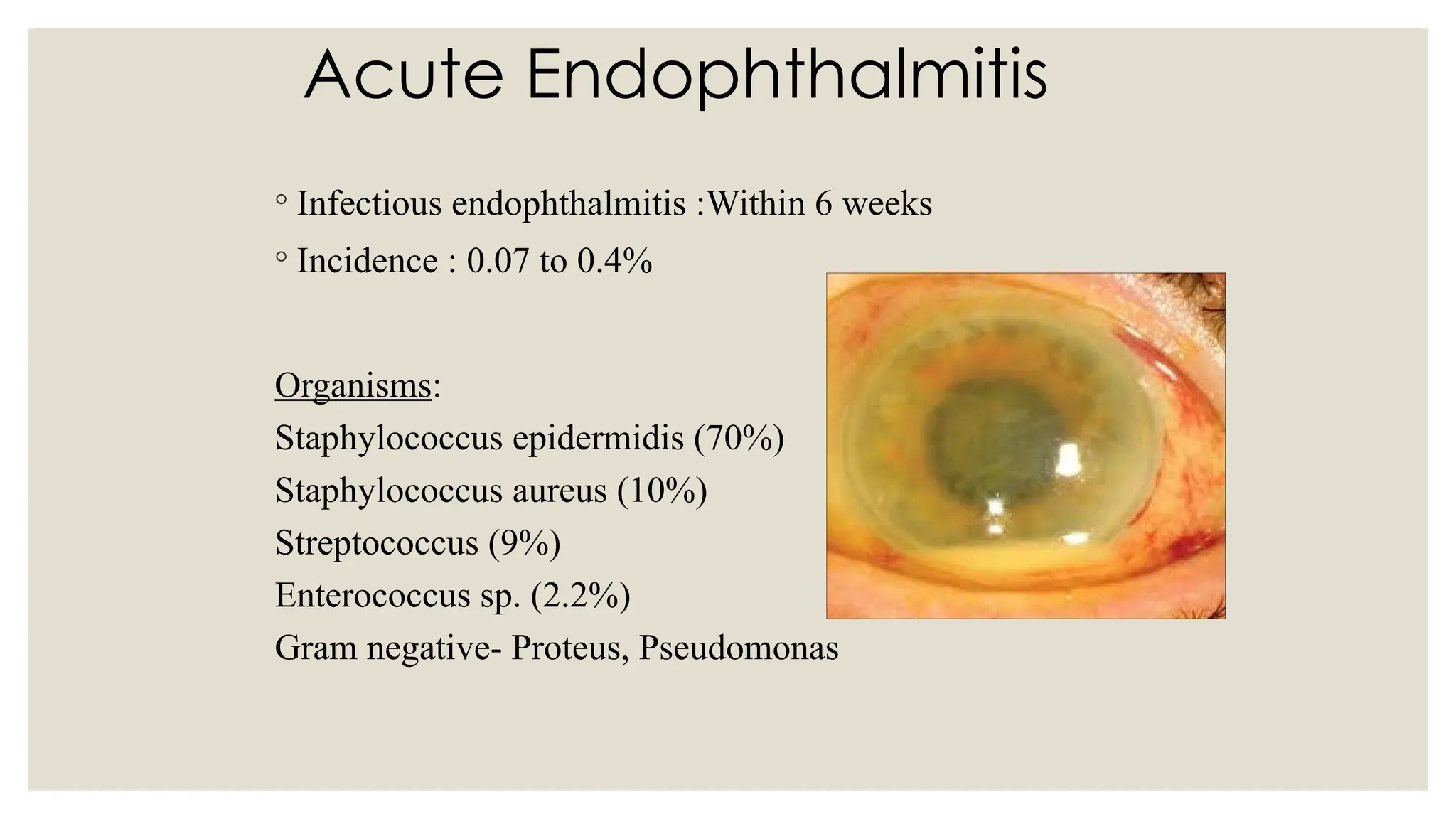
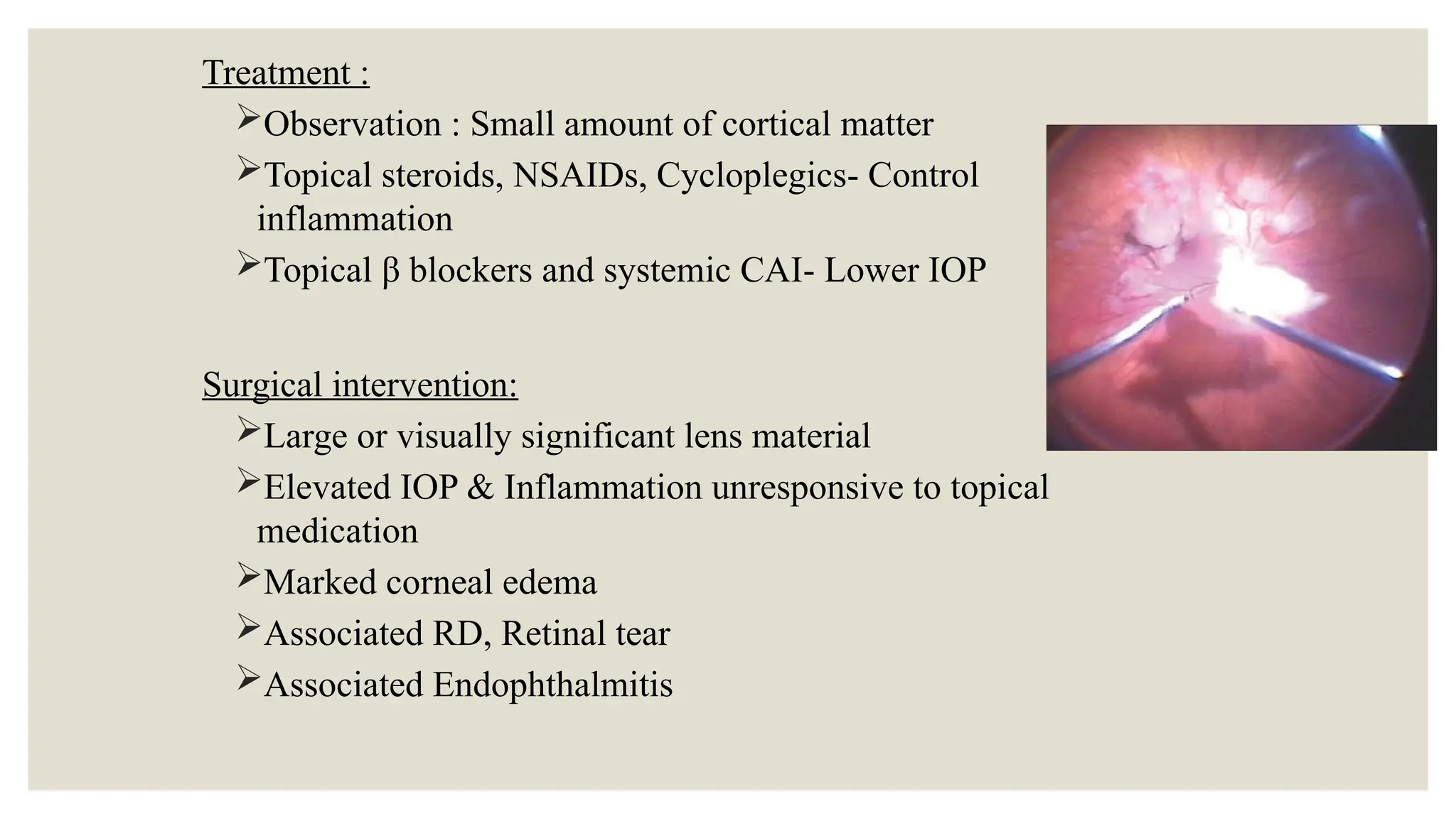
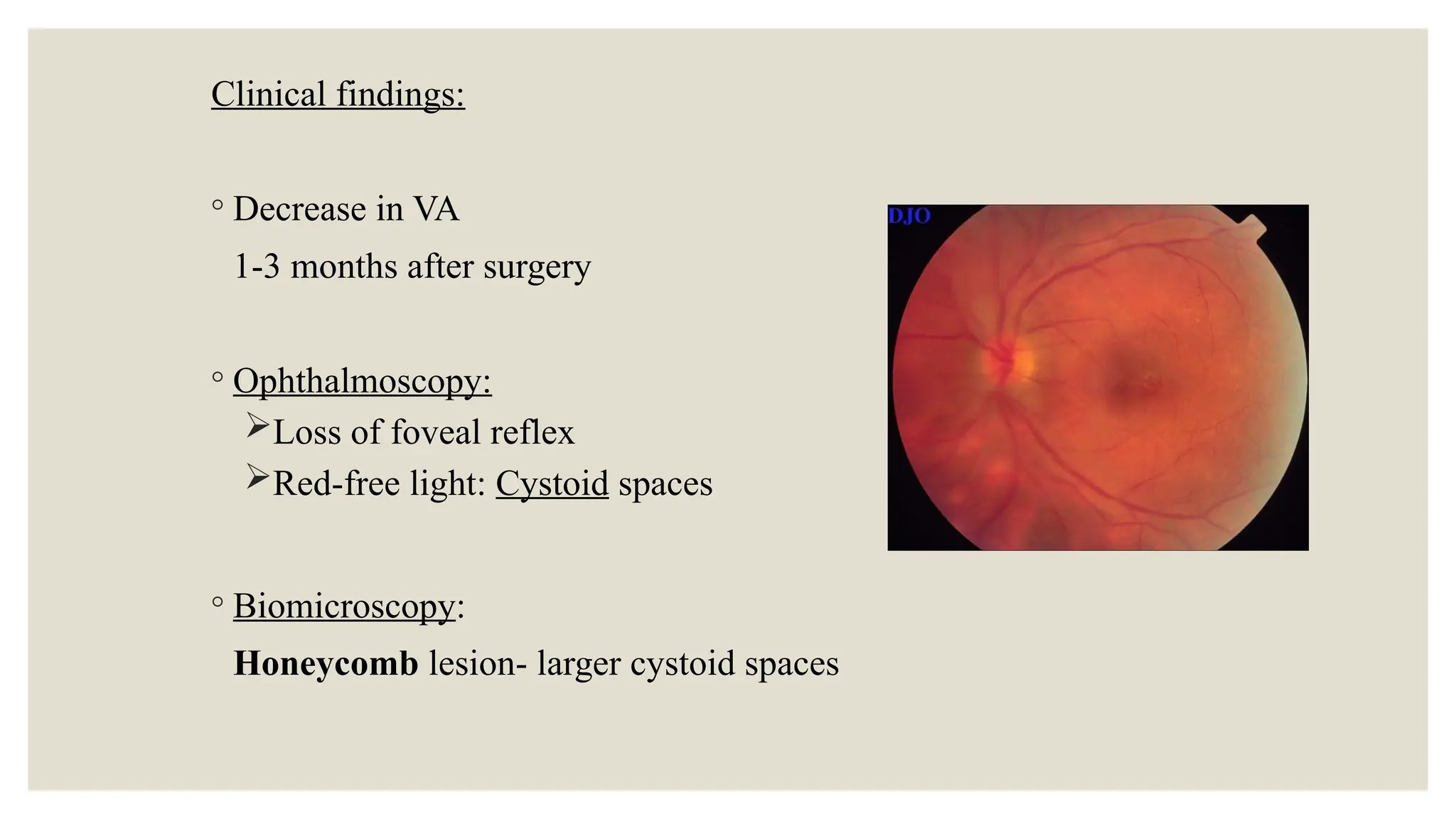
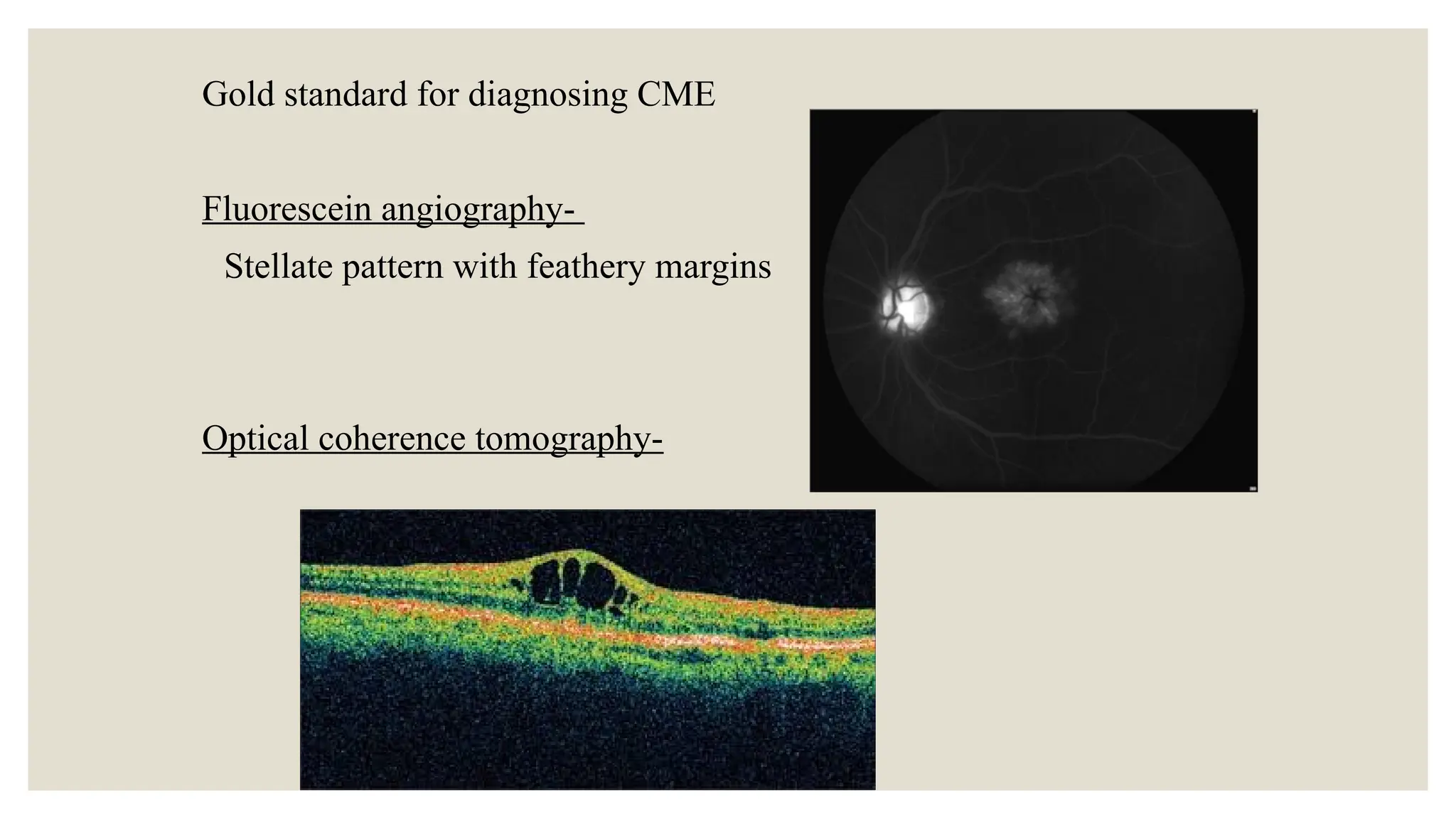
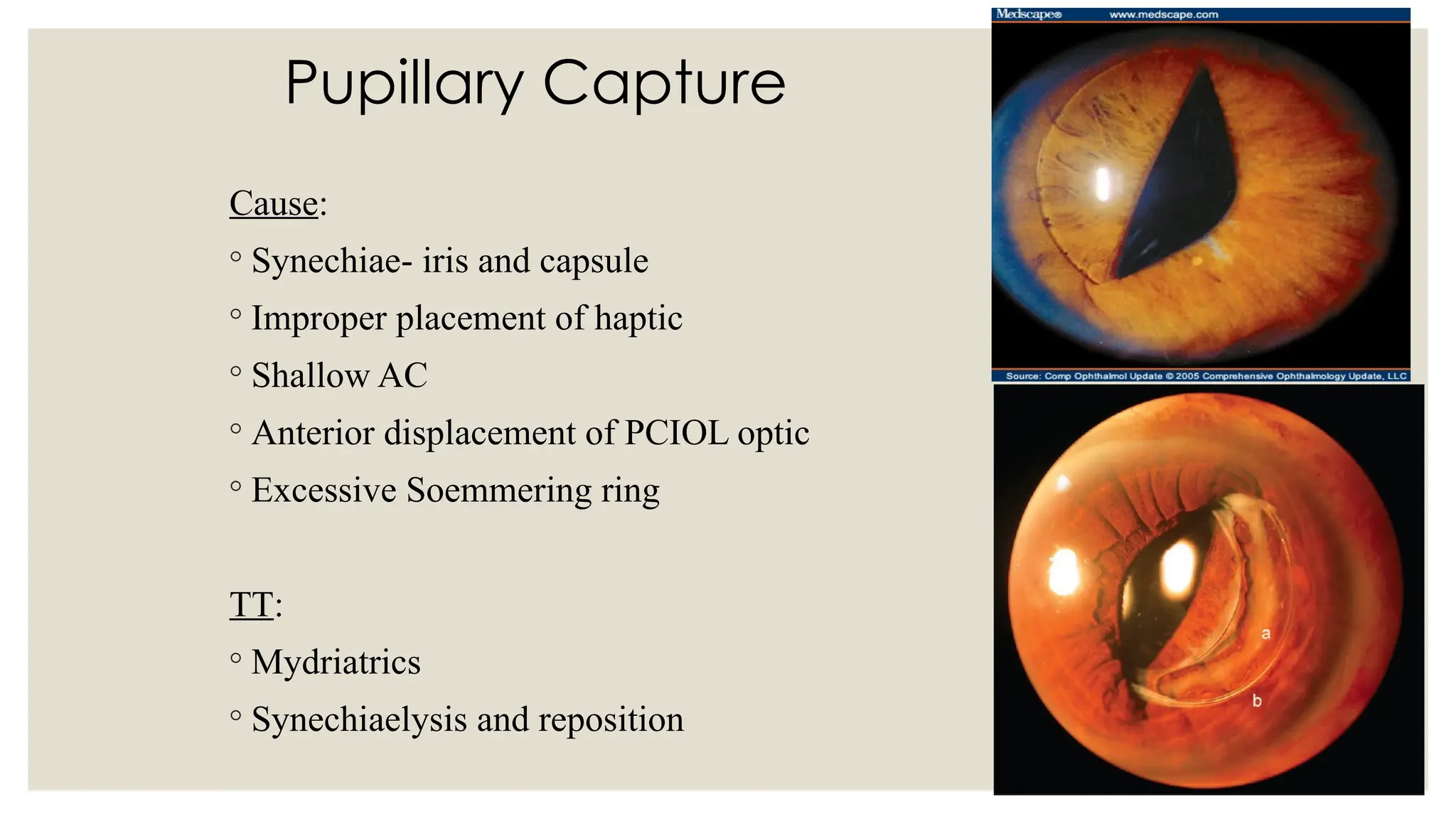
The document discusses various complications associated with cataract surgery, categorizing them into preoperative, intraoperative, postoperative, and intraocular lens (IOL) related complications. It outlines the risks, management strategies, and specific issues such as iris prolapse, anterior capsulotomy complications, and endophthalmitis, along with their respective treatments. Additionally, it covers complications arising from surgical techniques, postoperative glaucoma, and toxic anterior segment syndrome.