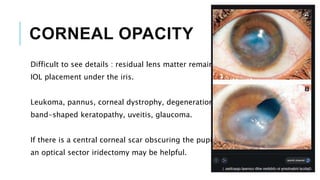
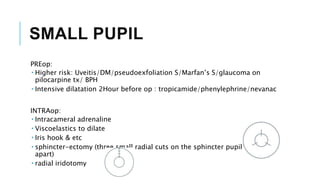
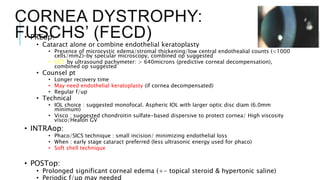
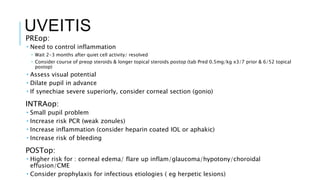
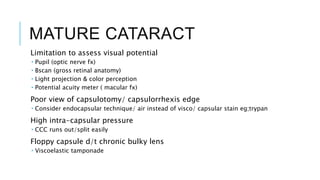
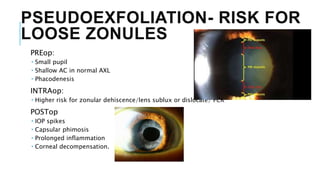
This document discusses special considerations for cataract surgery in situations with potential visualization problems or involvement of the anterior or posterior eye segments. It outlines challenges and recommendations for cases involving corneal opacities, small pupils, high myopia, corneal dystrophy, uveitis, mature cataracts, pseudoexfoliation, diabetes, glaucoma and other conditions. Key points addressed include preoperative assessment and preparation, intraoperative techniques, and postoperative management to help reduce risks and optimize outcomes for these more complex cases.