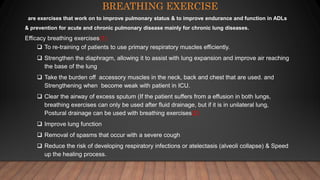
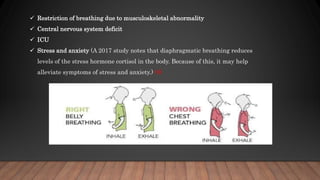
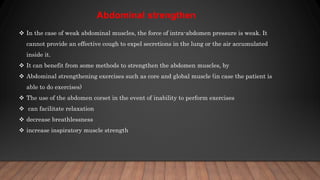
This document discusses various breathing exercises used in airway clearance therapy. It describes techniques like diaphragmatic breathing, pursed lip breathing, and segmental breathing. Diaphragmatic breathing aims to strengthen the diaphragm muscle and improve gas exchange. Pursed lip breathing is designed to make breaths more effective for those with lung conditions like COPD by slowing respiration. Segmental breathing consciously directs breathing to specific chest segments to promote lung expansion. Precautions and procedures are provided for safely performing these exercises.


























![Reference
1. https://www.ausmed.com/cpd/articles/breathing-exercises
2. Physiotherapy in Respiratory Care: An Evidence-based Approach to RespiratoryBMJ.
2018;360:j5916. Published 2018 Jan 24. doi:10.1136/bmj.j5916
3. https://www.slideshare.net/rahulapcvtp/breathing-exercise-rahul-ap-mpt
4. Boden I, Skinner EH, Browning L, et al. Preoperative physiotherapy for the prevention of
respiratory complications after upper abdominal surgery: pragmatic, double blinded,
multicentre randomised controlled trial [published correction appears in BMJ. 2019 Apr
25;365:l1862].
5. https://www.ausmed.com/cpd/articles/breathing-exercises
6. https://www.medicalnewstoday.com/articles/diaphragmatic-breathing#conditions-it-can-help-with
7. Prem V, Sahoo RC, Adhikari P. Effect of diaphragmatic breathing exercise on quality of life
in subjects with asthma: A systematic review. Physiother Theory Pract. 2013;29(4):271-277.
8. Ma X, Yue ZQ, Gong ZQ, et al. The Effect of Diaphragmatic Breathing on Attention,
Negative Affect and Stress in Healthy Adults. Front Psychol. 2017;8:874. Published 2017
Jun 6. doi:10.3389/fpsyg.2017.00874](https://image.slidesharecdn.com/breathingexerciesx-201225171534/85/Breathing-exercise-33-320.jpg)


