This document provides information on various breathing exercises including their goals, techniques, indications, and precautions. Key points include:
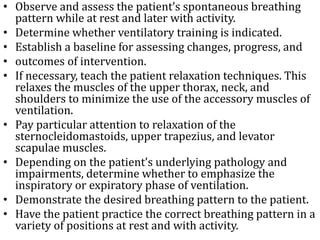
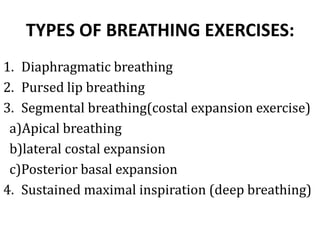
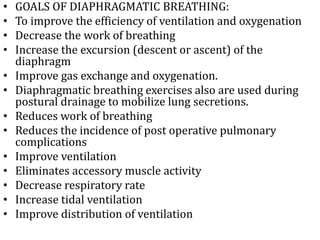
- Breathing exercises aim to improve pulmonary function and endurance through techniques like diaphragmatic breathing and pursed lip breathing.
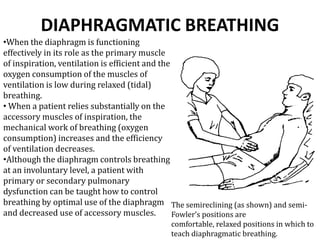
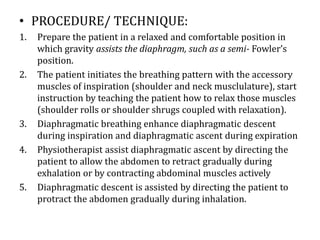
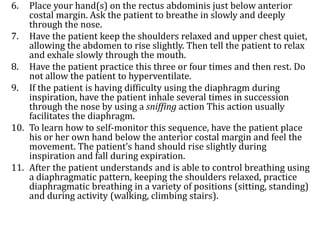
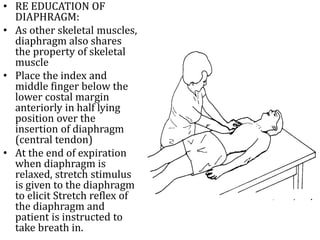
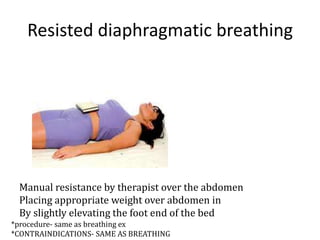
- Diaphragmatic breathing focuses on abdominal breathing to improve ventilation efficiency. Pursed lip breathing prolongs exhalation to slow breathing rate.
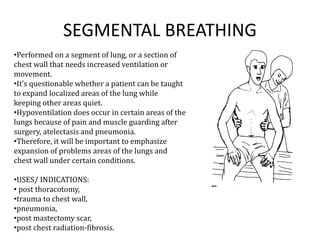
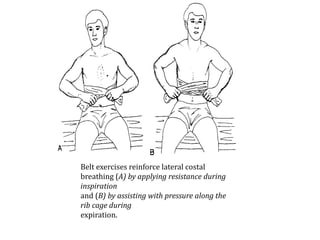
- Segmental breathing targets specific lung areas for those with issues post-surgery or illness.
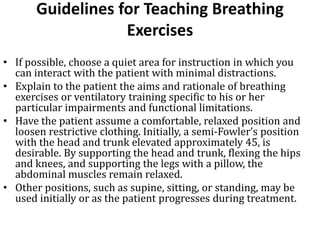
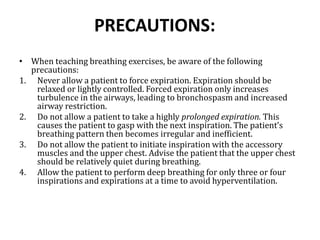
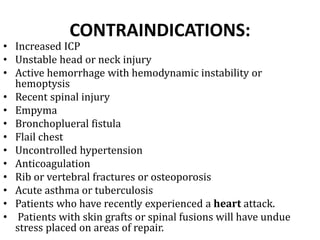
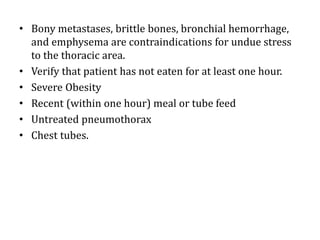
- Indications for breathing exercises include COPD, cystic fibrosis, pneumonia, and other pulmonary disorders. Precautions aim to avoid hyperventilation or forced breathing.