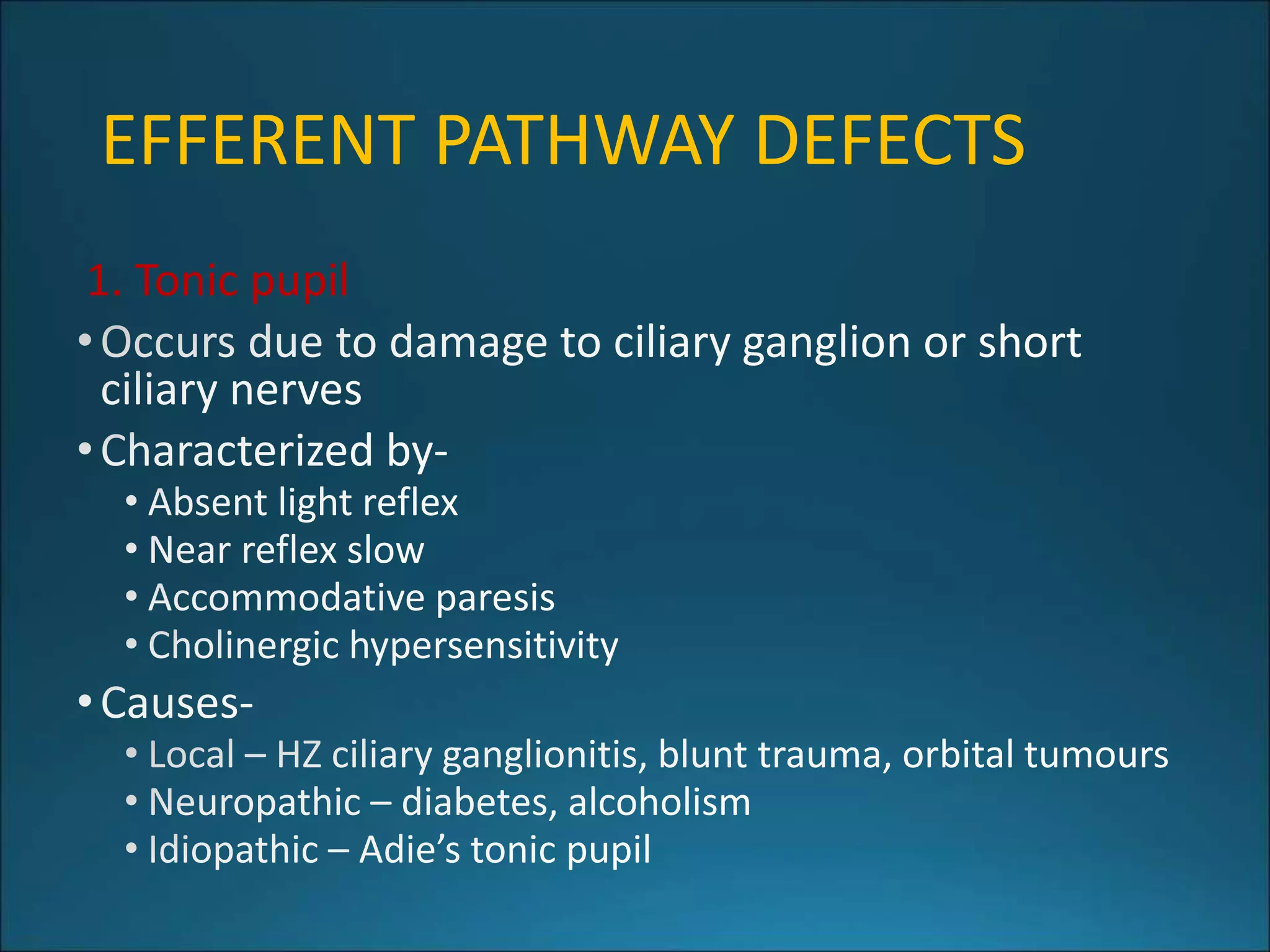
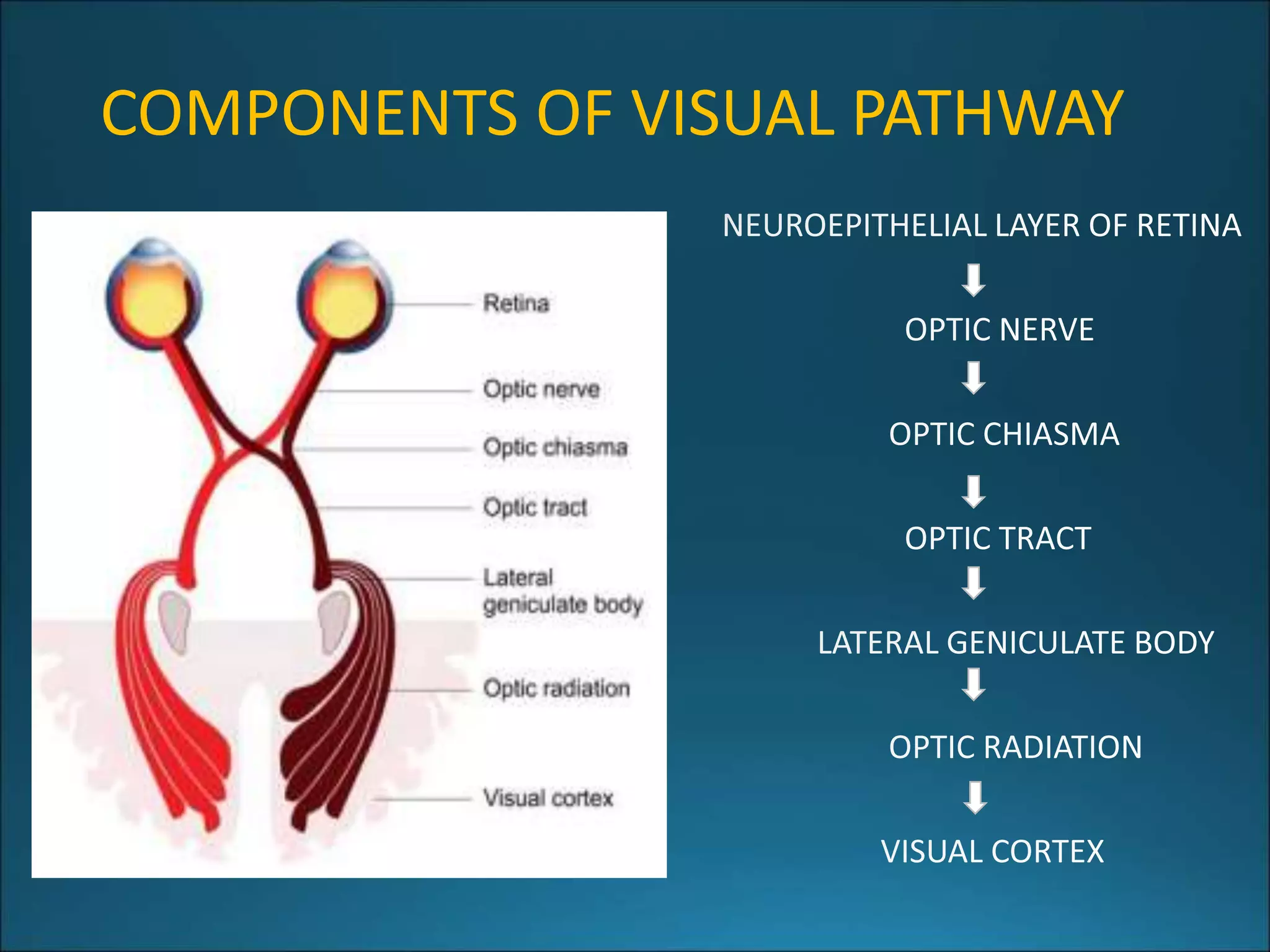
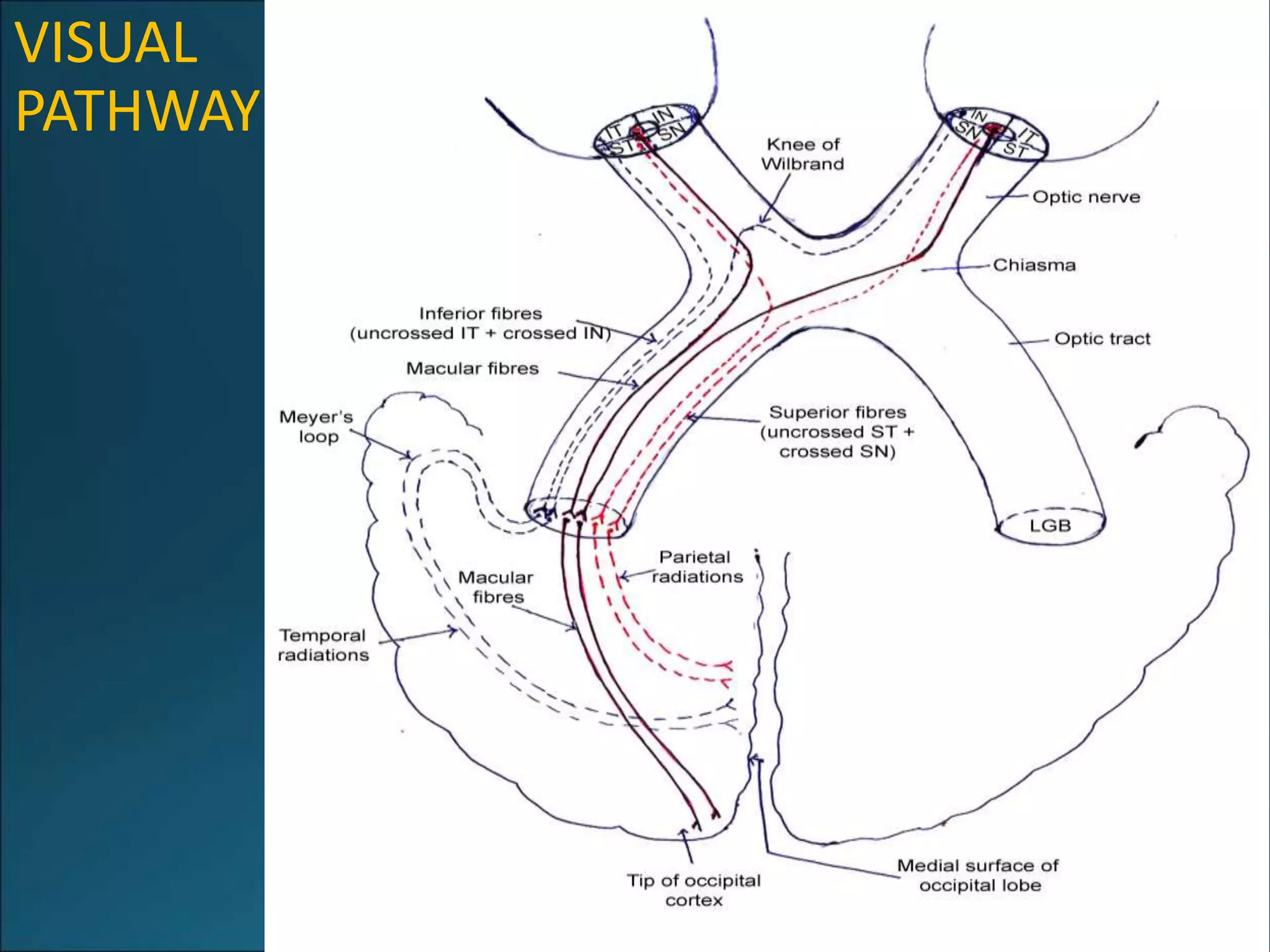
1. The visual pathway includes the optic nerve, optic chiasm, optic tracts, lateral geniculate bodies, and optic radiations which transmit visual information from the eyes to the visual cortex.
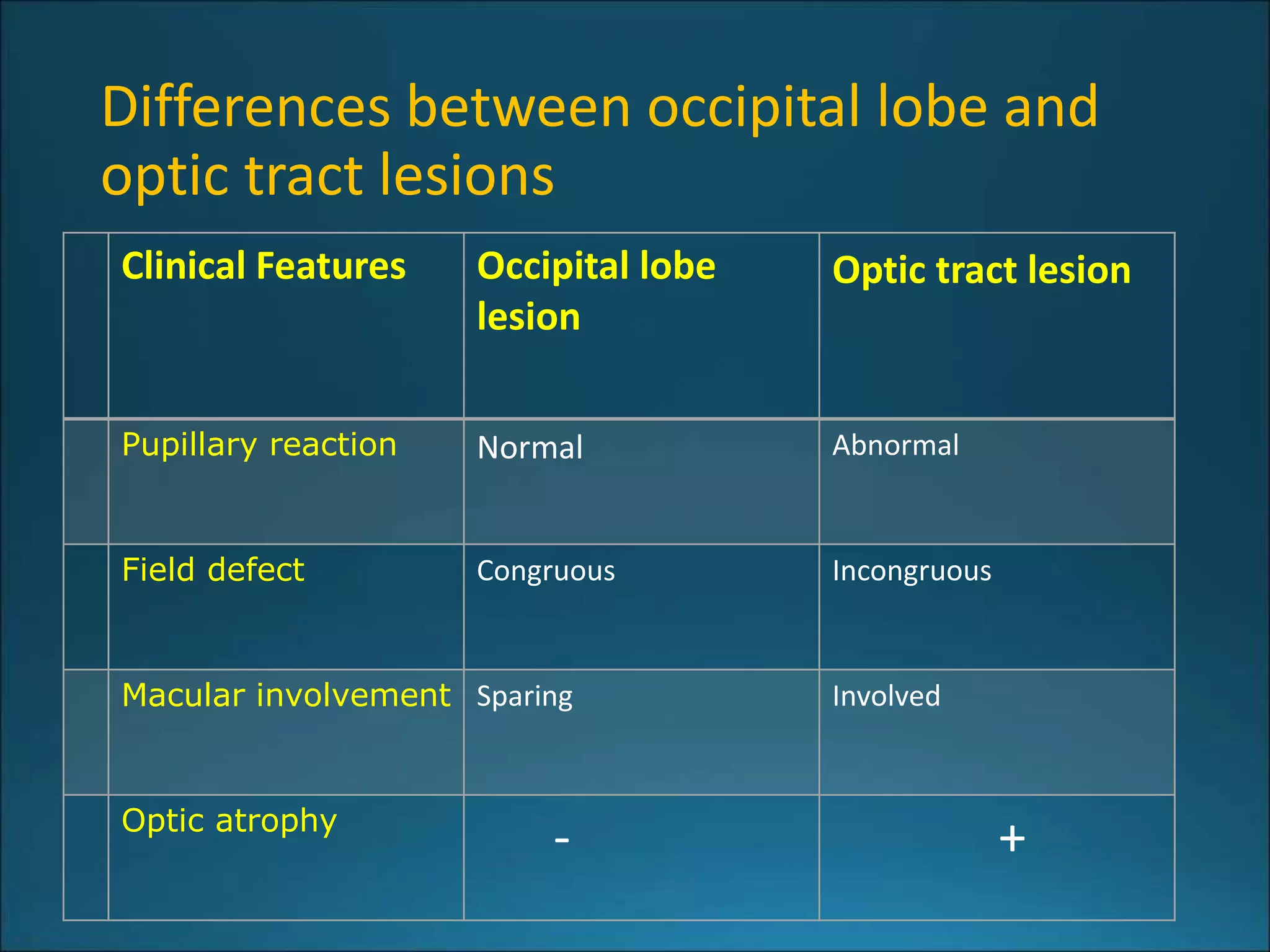
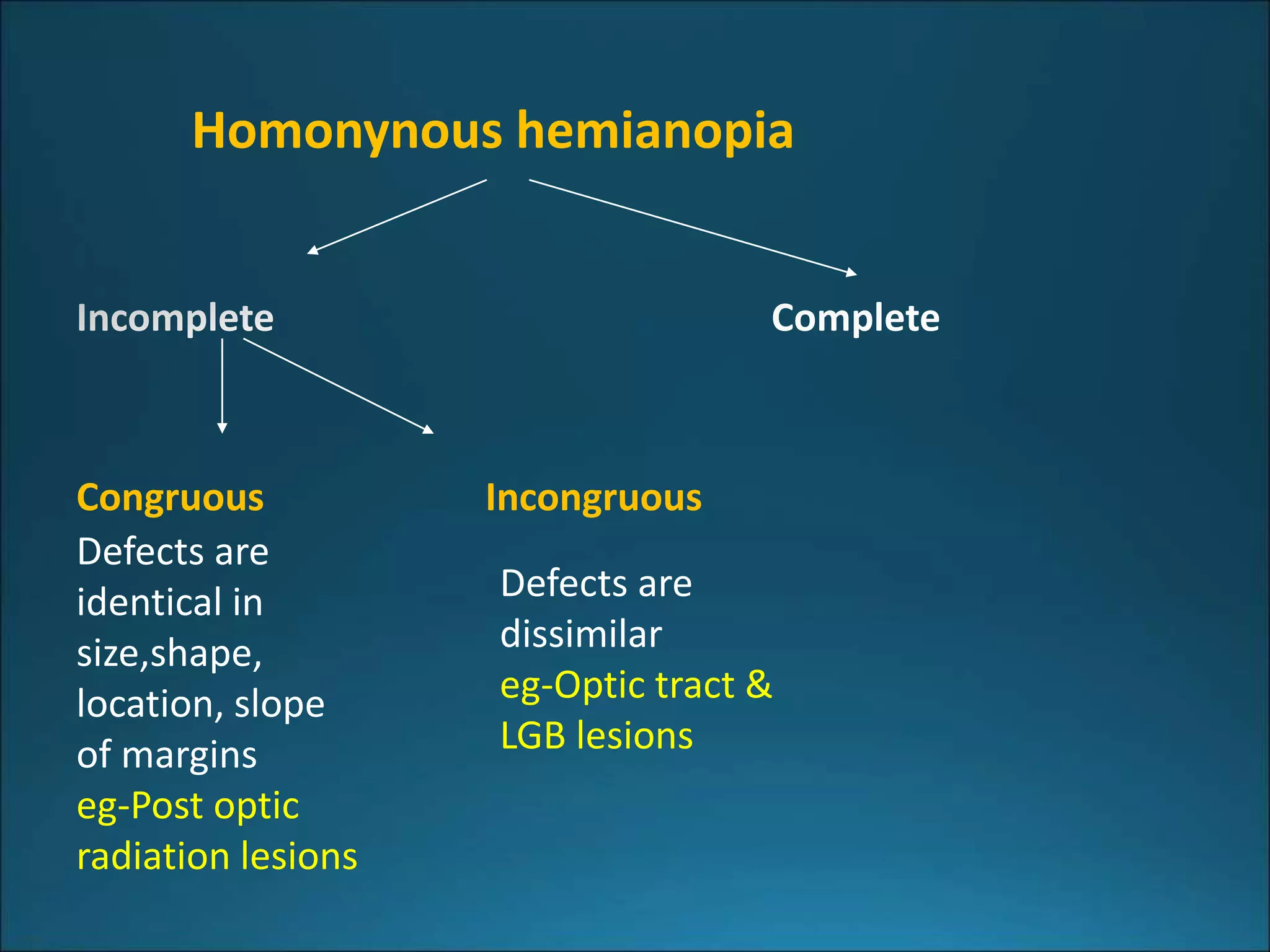
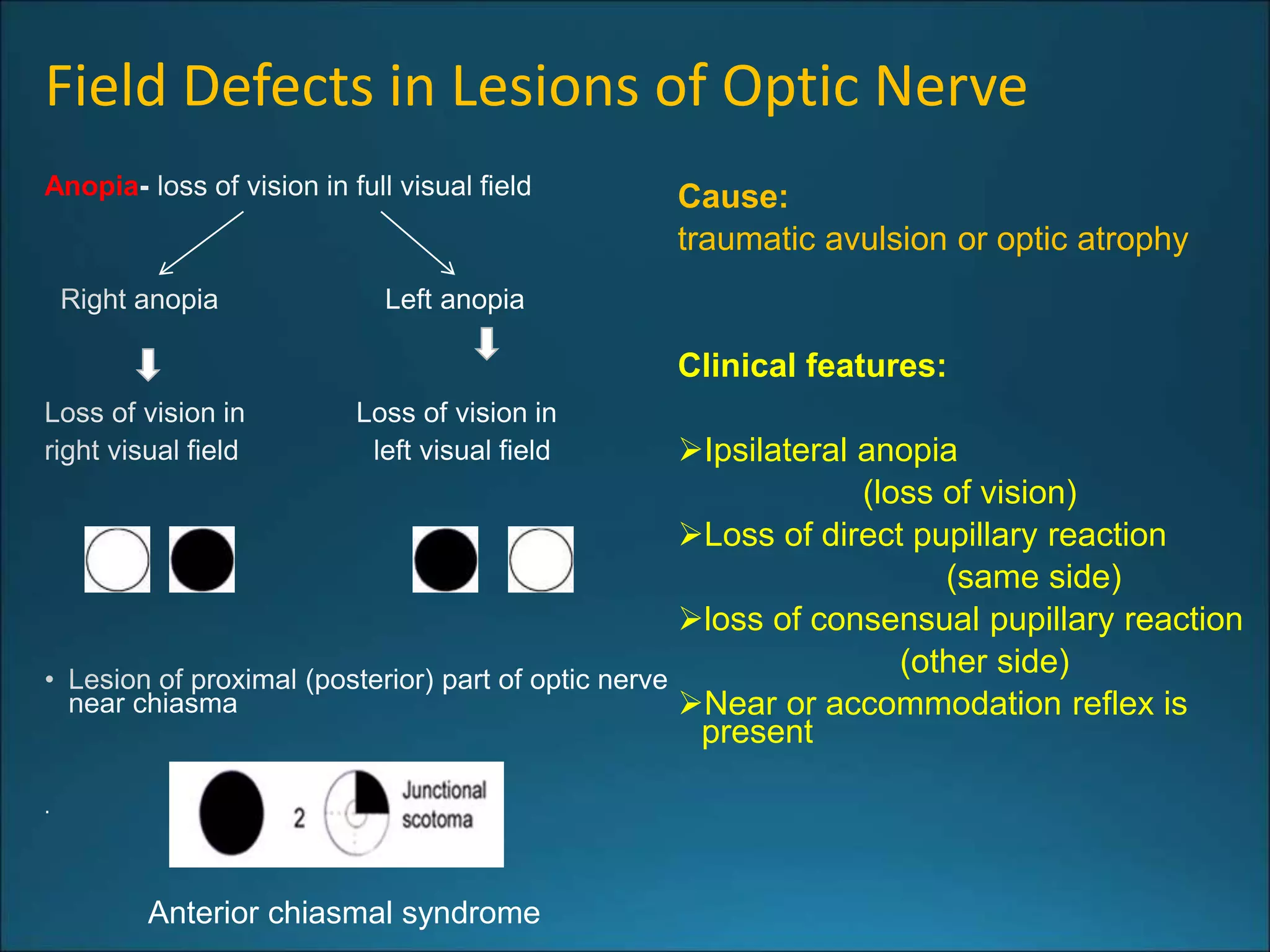
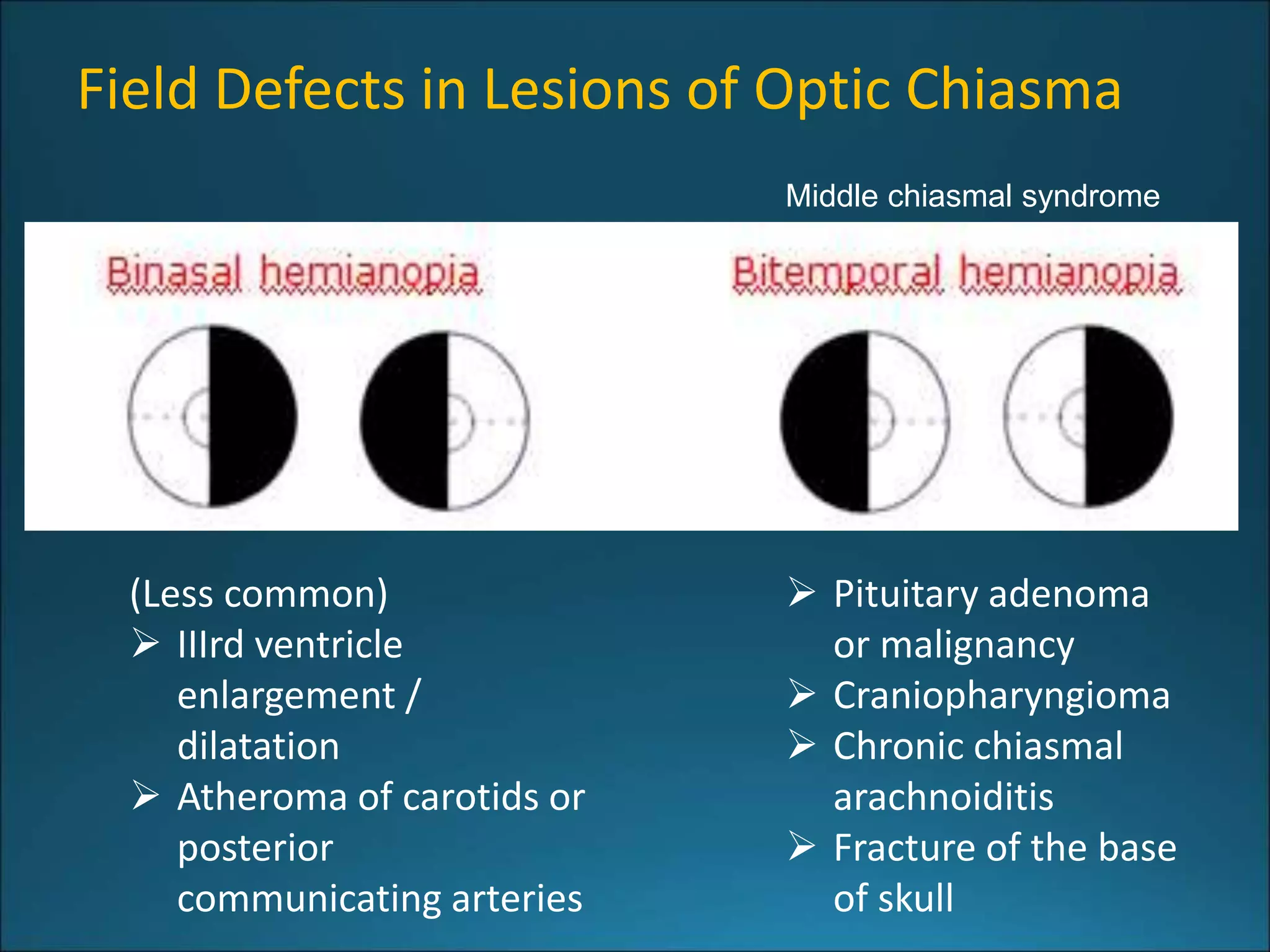
2. Lesions along the visual pathway can cause different types of visual field defects including hemianopia, quadrantanopia, and homonymous hemianopia. The type and characteristics of the field defect depend on the specific location of the lesion.
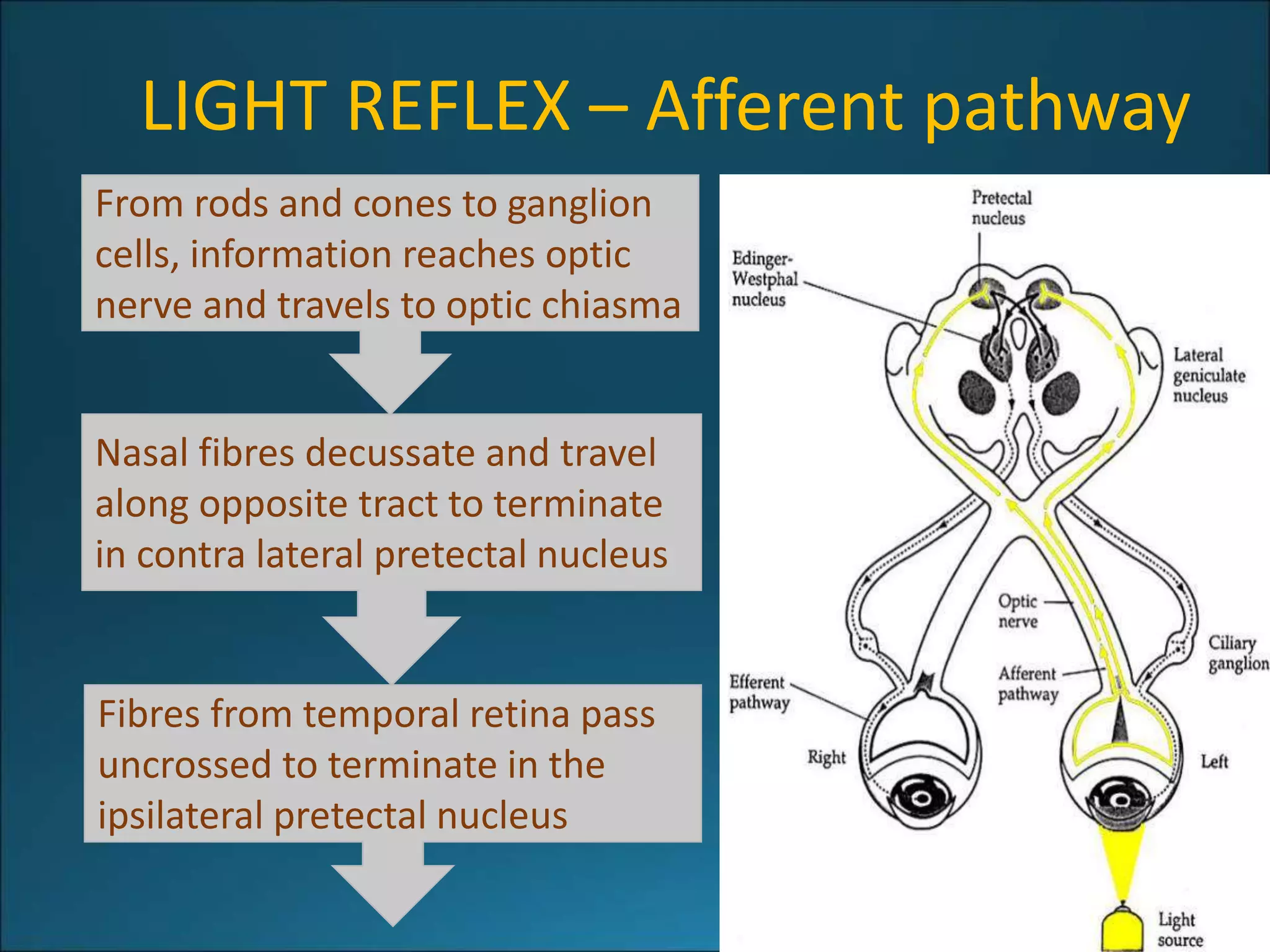
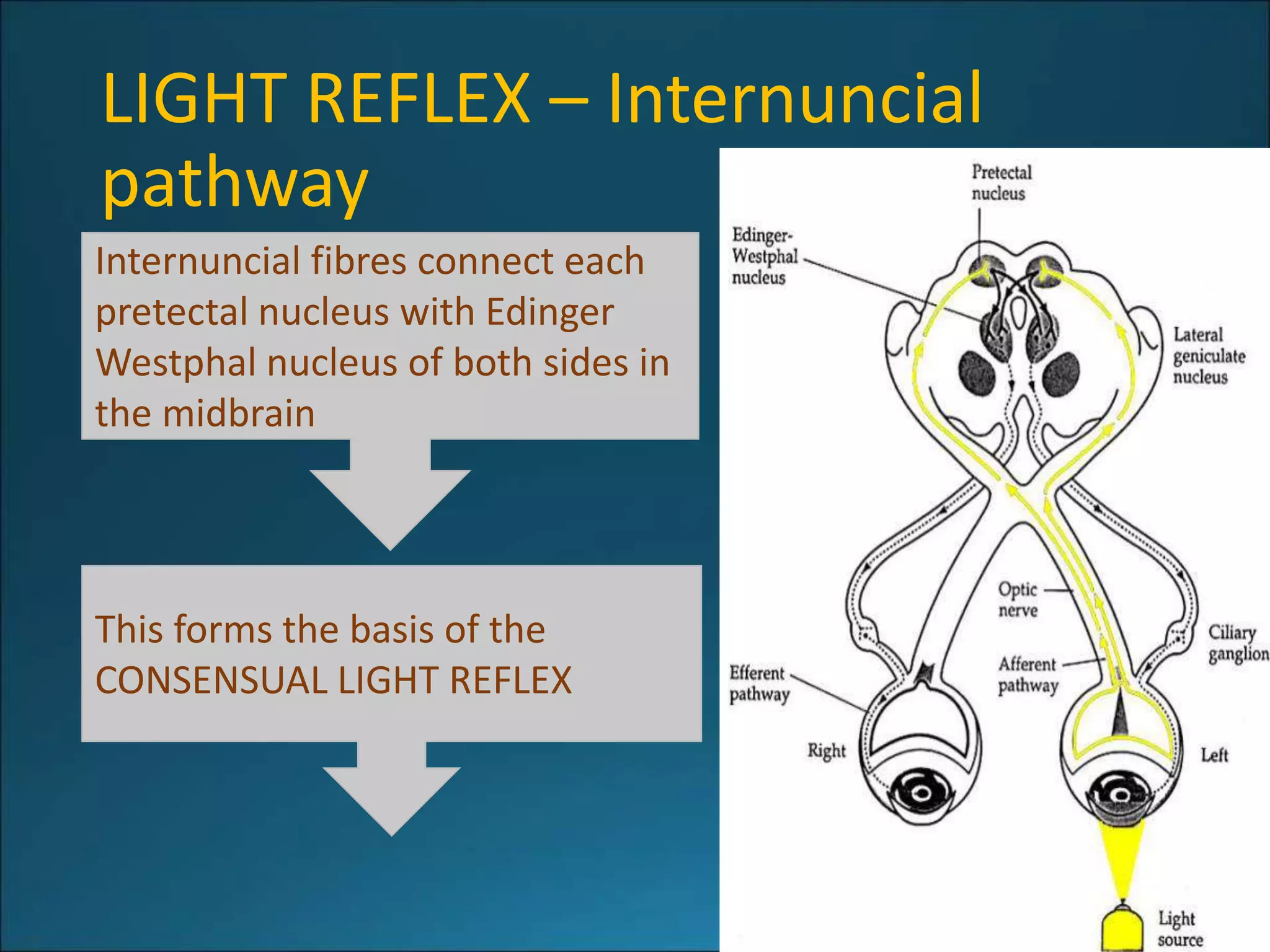
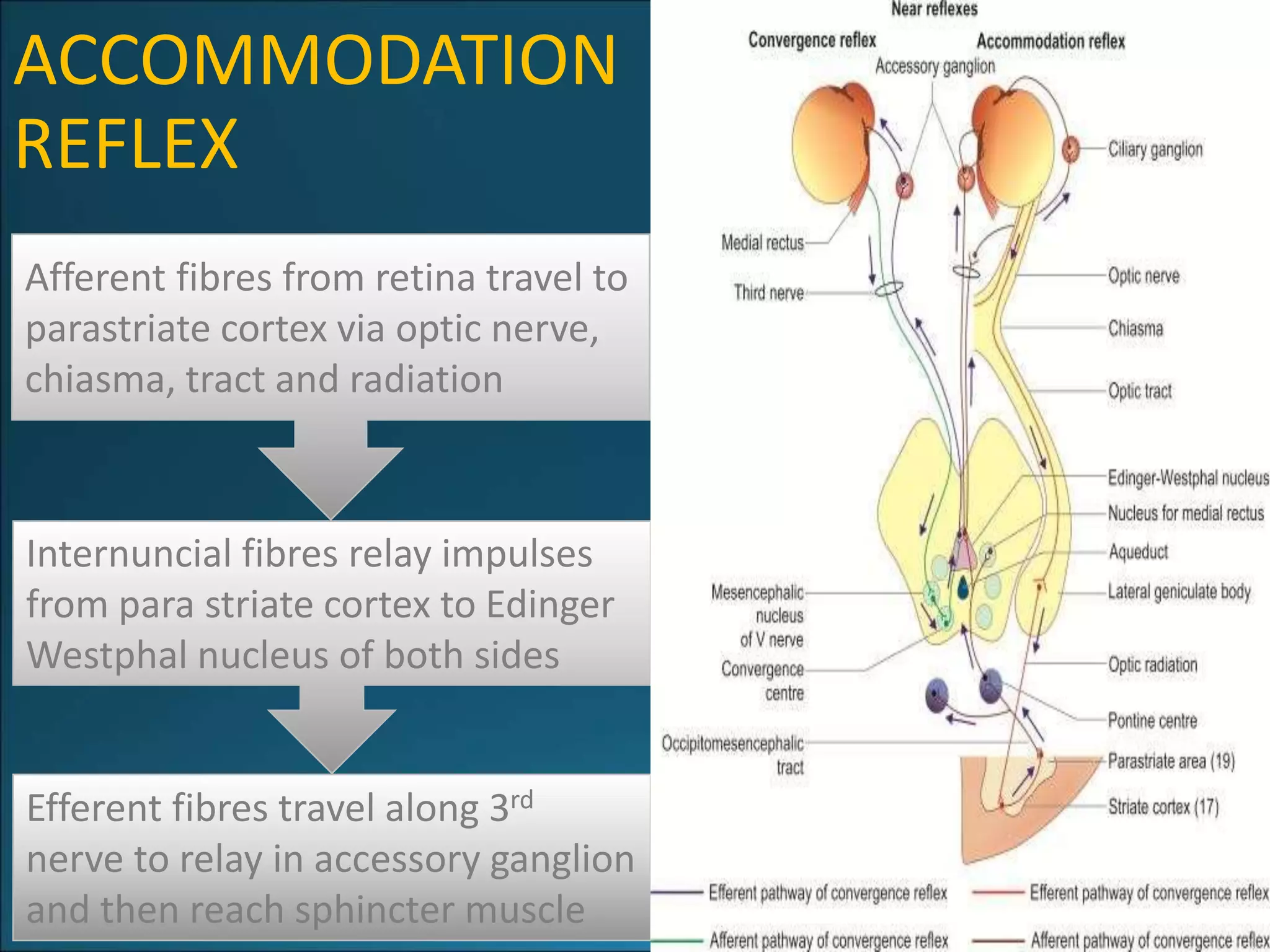
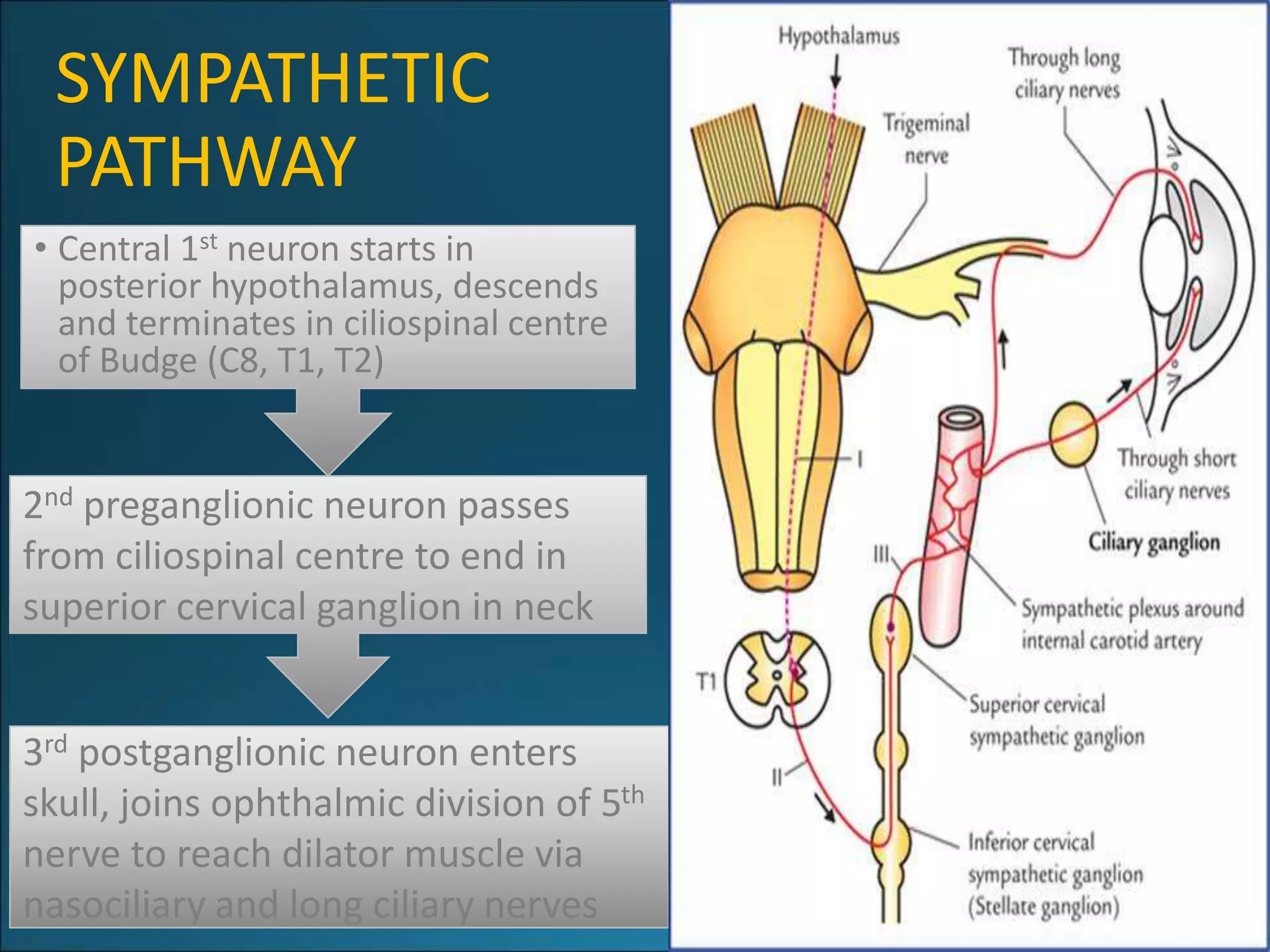
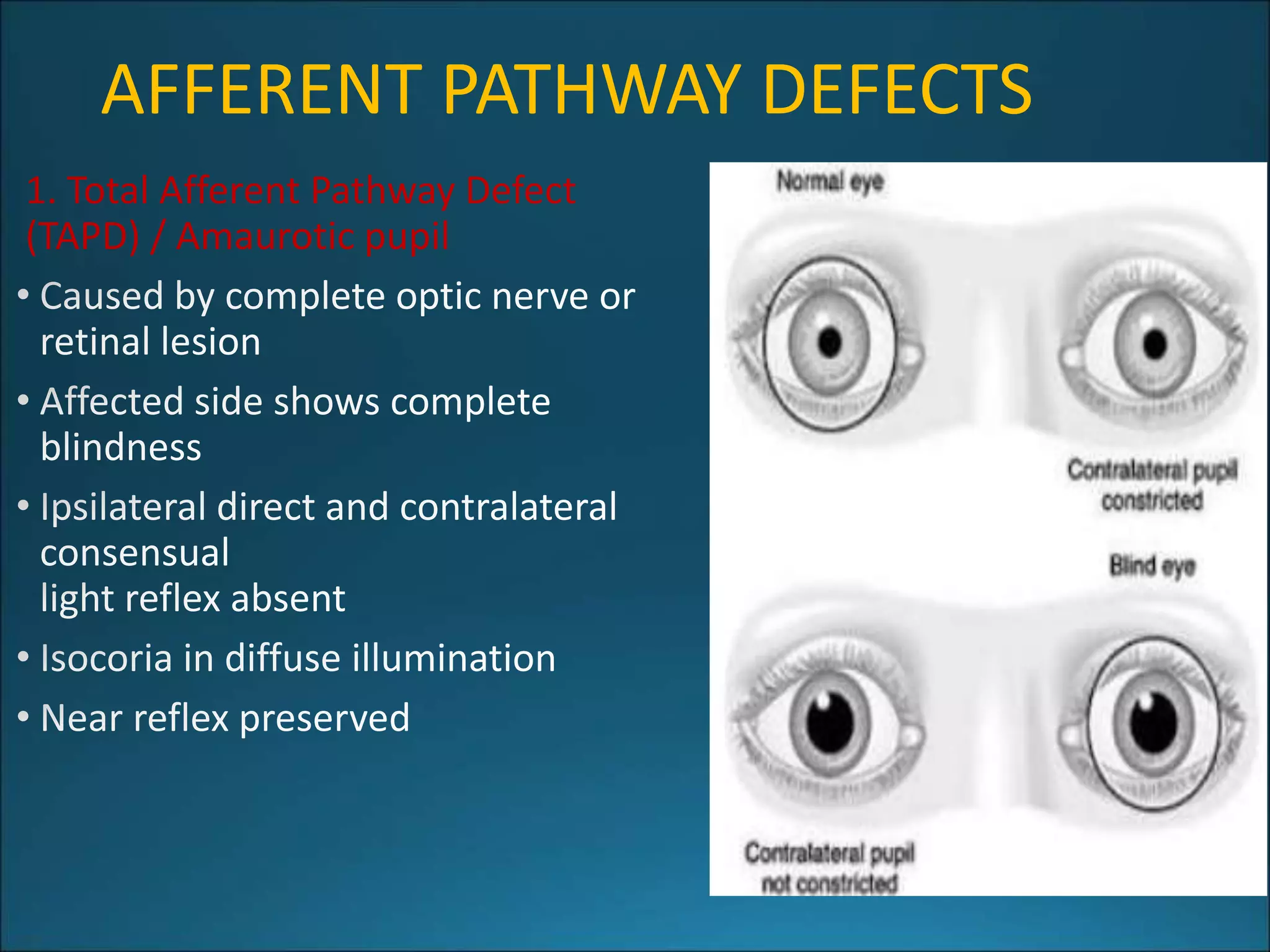
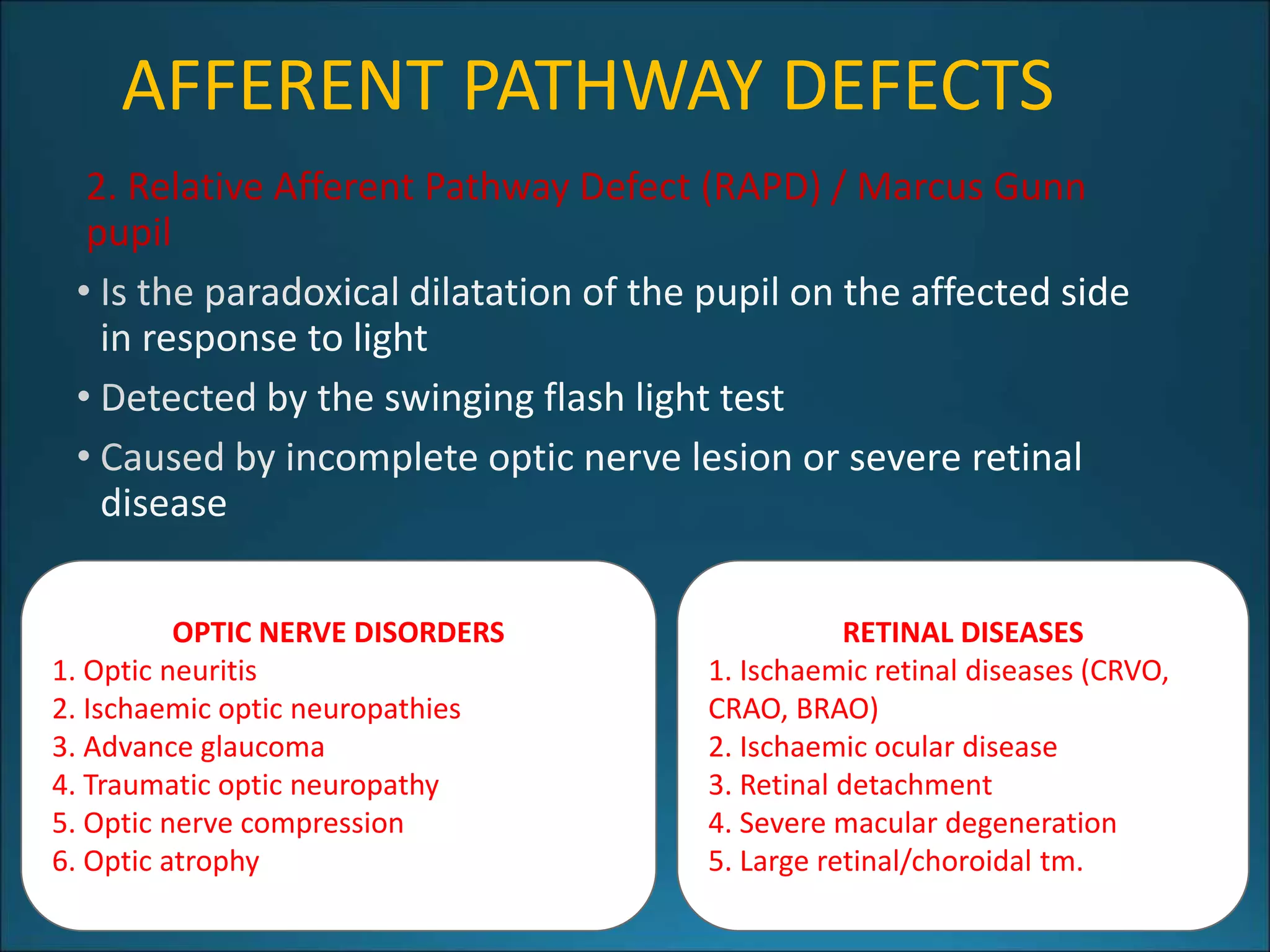
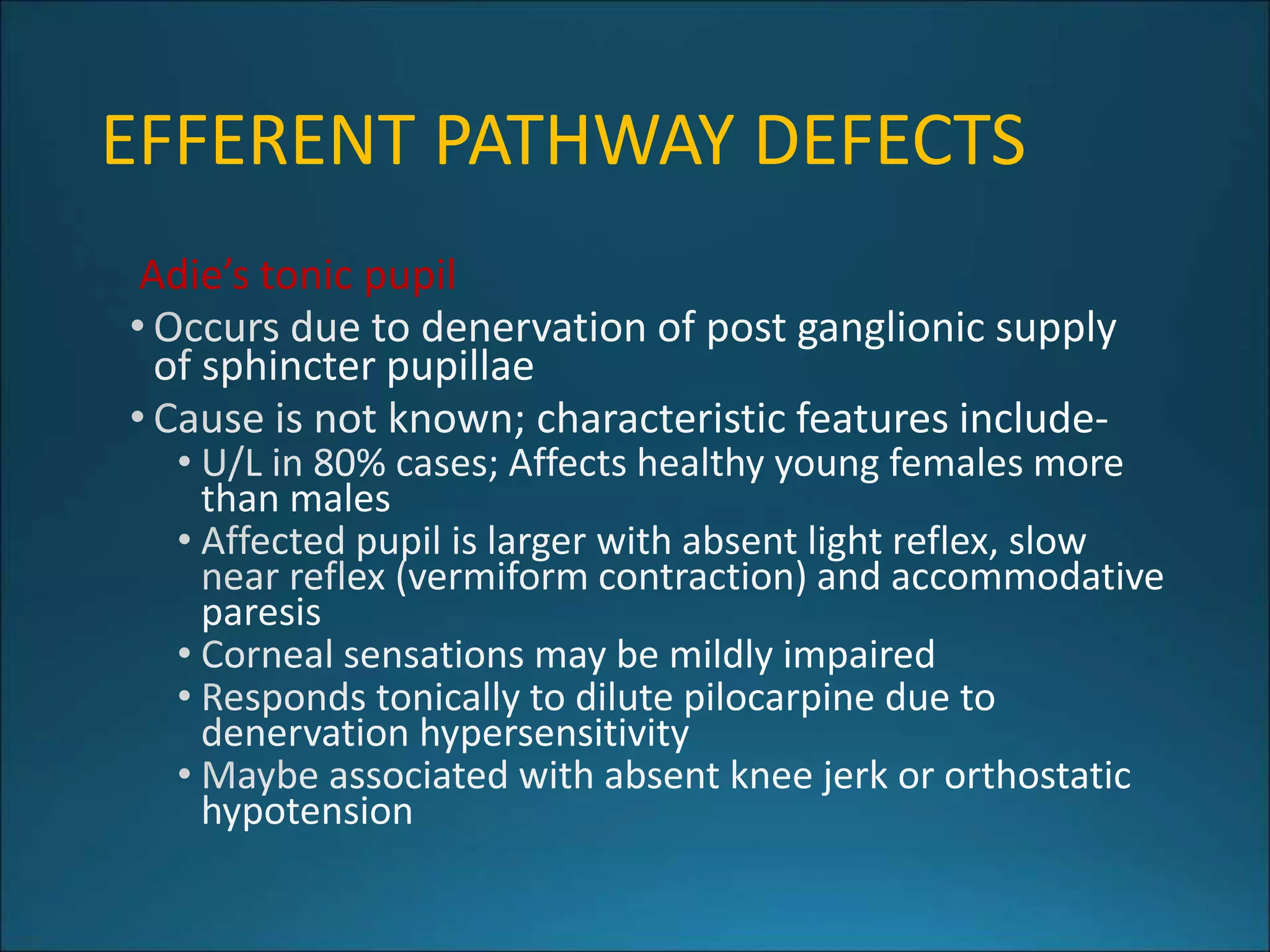
3. Pupillary reflexes involve both afferent and efferent pathways. Abnormalities of the pupillary reflexes can localize lesions and help diagnose conditions affecting the visual pathway or autonomic nervous system.














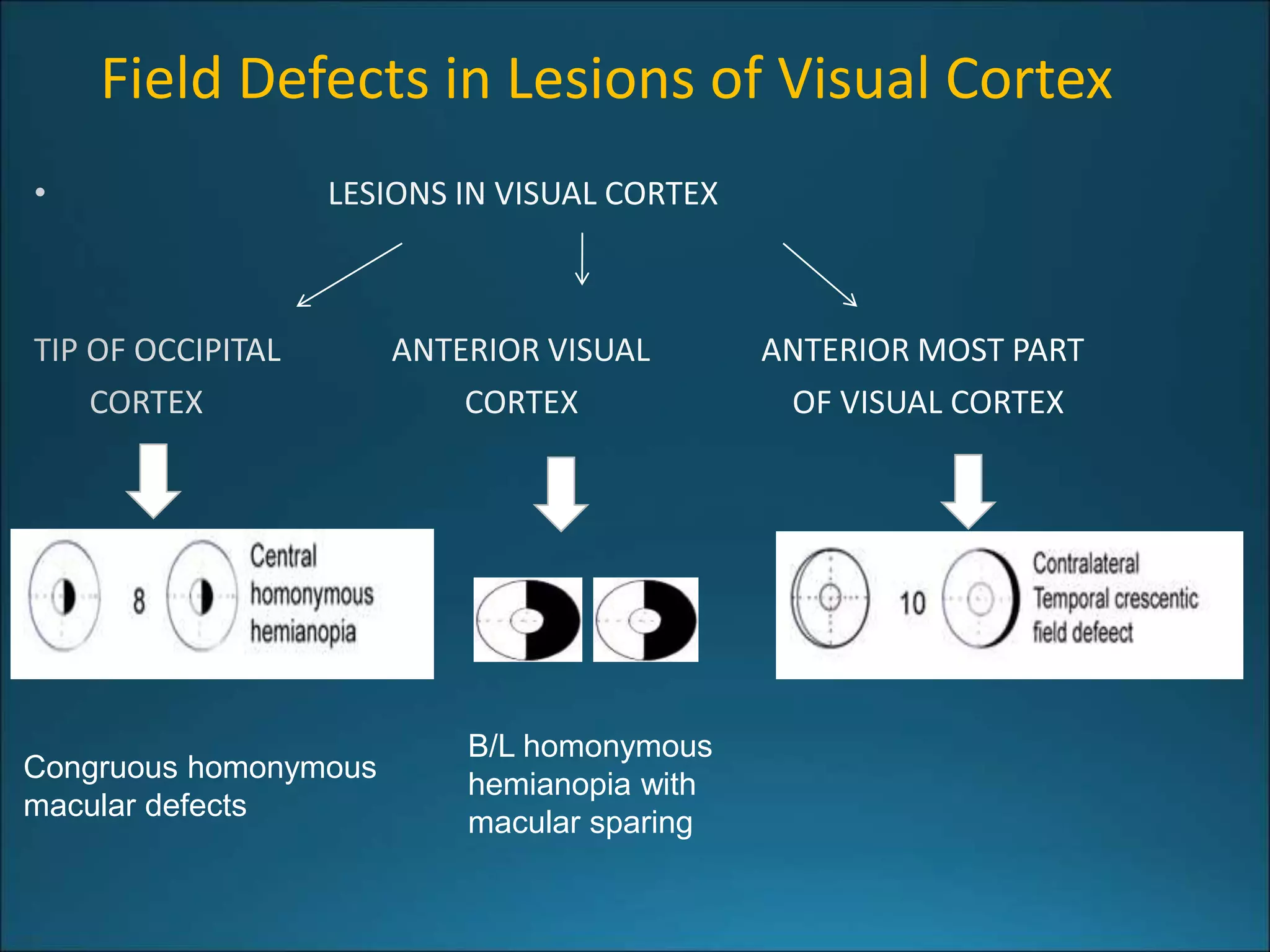
![Clinical presentation in Visual Cortex
Lesions (Cortical blindness)
[Anton syndrome]
[Riddoch phenomenon]
[Alexia]](https://image.slidesharecdn.com/734visualpathwaylesions-230523135538-e24d2560/75/734_Visual_Pathway_lesions-pptx-23-2048.jpg)