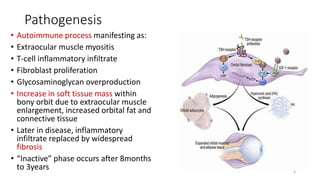
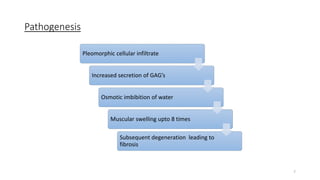
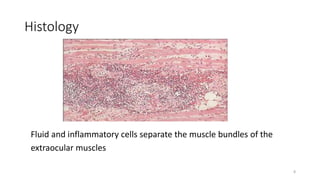
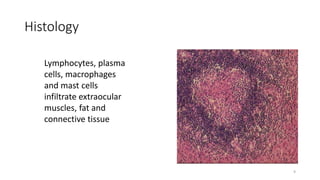
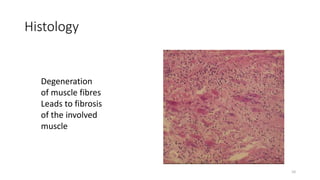
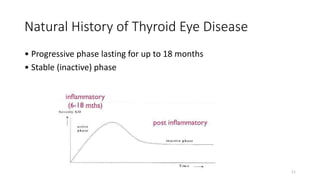
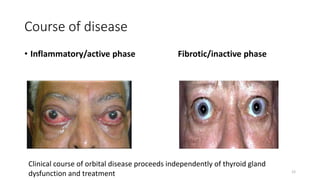
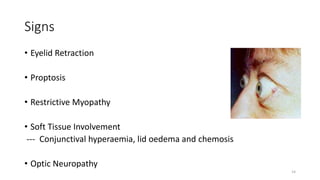
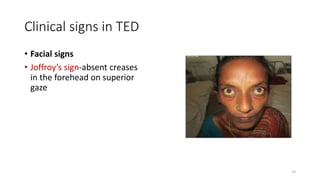
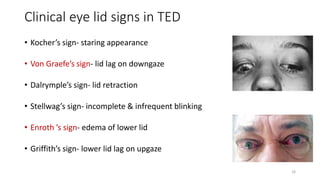
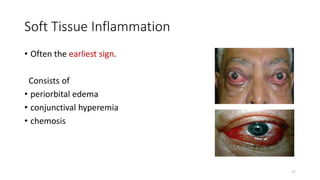
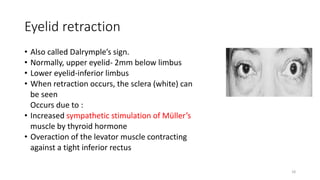
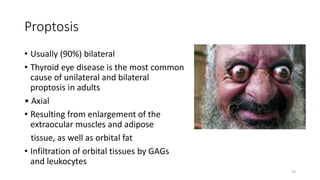
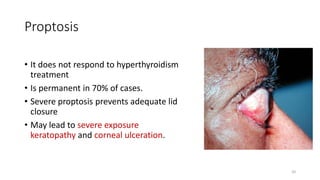
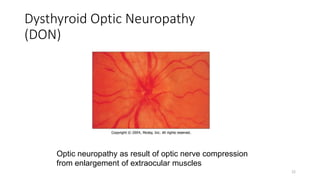
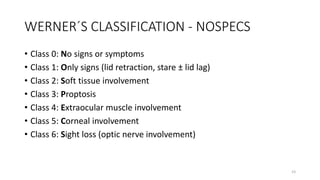
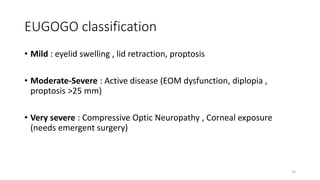
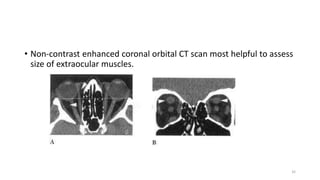
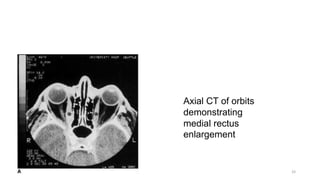
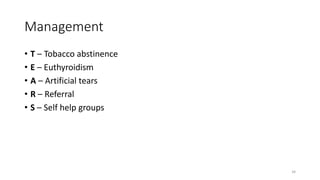
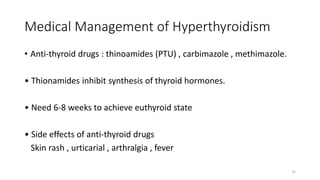
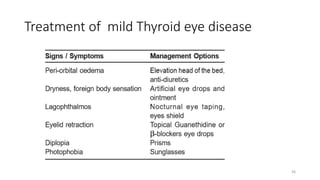
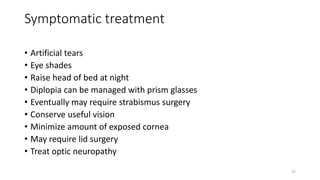
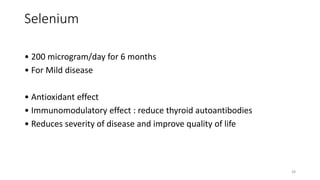
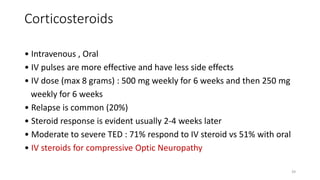
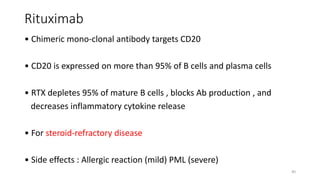
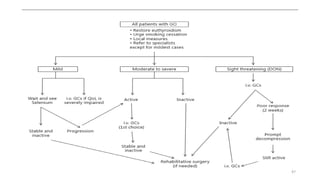
This document provides an overview of thyroid ophthalmopathy (TED), also known as Graves' ophthalmopathy. It discusses the epidemiology, etiology, risk factors, pathogenesis, clinical signs and symptoms, diagnosis, and management of the autoimmune disease. TED is caused by inflammation and accumulation of fluids in the orbit, raising pressure and causing enlargement of the extraocular muscles and adipose tissue. Symptoms include eye bulging, double vision, and dryness. Management involves treating any thyroid abnormalities, using corticosteroids, radiation, or surgery to address eye involvement and symptoms.